Drug Interactions: What You Need to Know Before Taking Multiple Medications
When you take more than one medication, your body doesn’t just see them as separate pills—it sees a drug interaction, a change in how one drug affects another when taken together. Also known as medication interaction, it can make a drug stronger, weaker, or cause unexpected side effects you never saw coming. This isn’t just about prescription drugs. It’s also about the over-the-counter drugs, medicines you buy without a prescription like pain relievers, cold pills, or antacids you grab off the shelf, and even the supplement interactions, natural products like vitamins, herbs, or fish oil that can still change how your body handles medicine you take daily. Many people think if it’s natural or sold without a prescription, it’s harmless. That’s not true. A common antihistamine like Benadryl can make your blood pressure meds less effective. A calcium supplement might block your thyroid medicine from being absorbed. And mixing alcohol with certain painkillers? That’s a one-way ticket to the ER.
Drug interactions don’t always cause obvious symptoms right away. Sometimes, they quietly reduce how well your medicine works. You might think your blood pressure isn’t dropping because the pill isn’t strong enough—but it’s actually being canceled out by your antacid. Or maybe your sleep aid isn’t helping, not because it’s weak, but because your antidepressant is fighting it. These aren’t rare edge cases. They happen every day. The FDALabel database shows over 149,000 drug labels list potential interactions, and many of them involve common combinations people don’t even think twice about. That’s why reading your label isn’t enough—you need to understand what’s happening behind the scenes. If you’re on gabapentin for nerve pain, taking it with a muscle relaxant could make you dangerously sleepy. If you’re using tadalafil for erectile dysfunction and also take nitroglycerin for heart issues, that combo can crash your blood pressure to life-threatening levels. Even something as simple as grapefruit juice can interfere with more than 85 medications, including statins and some blood pressure drugs. It’s not about being paranoid. It’s about being informed.
You don’t need to memorize every possible combo. But you do need to know how to protect yourself. Keep a list of everything you take—prescriptions, OTCs, supplements, even herbal teas. Bring it to every doctor visit. Ask your pharmacist: "Could any of these mess with each other?" Don’t assume your doctor knows about every supplement you take. Most don’t. And if you notice something off—unusual dizziness, sudden fatigue, a rash, or your usual meds just not working—that’s not normal. It could be a hidden interaction. The posts below cover real cases: how antihistamines worsen restless legs, how calcium affects thyroid meds, why certain painkillers shouldn’t mix with blood thinners, and what to do if you accidentally combine meds that shouldn’t be together. These aren’t theory. These are stories from people who learned the hard way. And now you can learn from them before it’s too late.
 3 January 2026
3 January 2026
Green Tea Extract and Medication Interactions to Watch
Green tea extract may seem harmless, but it can dangerously reduce the effectiveness of medications like blood pressure drugs, statins, and chemotherapy. Learn which interactions are life-threatening and how to stay safe.
 18 November 2025
18 November 2025
Pharmacokinetic vs Pharmacodynamic Drug Interactions: What You Need to Know
Learn how pharmacokinetic and pharmacodynamic drug interactions work, why they matter for safety, and what you can do to avoid dangerous side effects when taking multiple medications.
Latest Posts
-

How to Buy Cheap Generic Accutane (Isotretinoin) Online Safely
-

Imipramine and Diet: Foods to Eat and Avoid for Better Mental Health
-
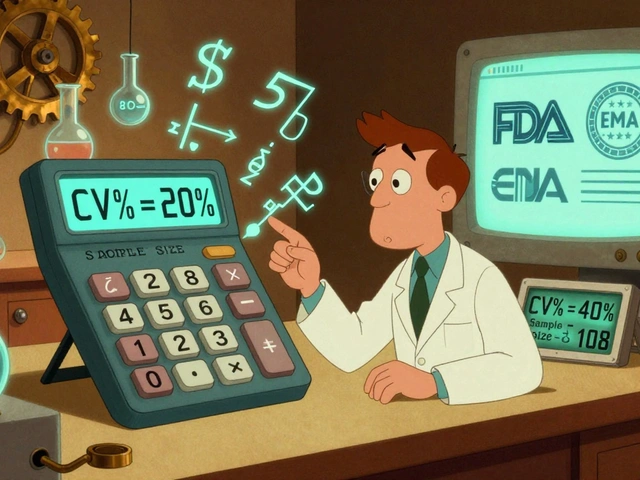
Statistical Analysis in BE Studies: How to Calculate Power and Sample Size Correctly
-

DOAC Dosing in Obesity: What You Need to Know About Efficacy, Safety, and Side Effects
-

Depression Management: Medications, Therapy, and Lifestyle Changes That Work

15