DOAC Dosing Calculator for Obesity
Patient Profile
DOAC Recommendations
When you’re managing blood clots or atrial fibrillation and you’re living with obesity, the question isn’t just which blood thinner to use-it’s how much. Direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, dabigatran, and edoxaban were designed to be simpler than warfarin: fixed doses, no routine blood tests, fewer food interactions. But when a patient weighs over 120 kg or has a BMI above 40 kg/m², does that simplicity still hold up?
Why Obesity Changes the Game
Obesity isn’t just about weight. It changes how drugs move through the body-absorption, distribution, metabolism, and elimination. The original clinical trials for DOACs included very few patients with morbid obesity. That gap created real uncertainty. If a drug is cleared faster or distributed more widely in a larger body, could the standard dose be too low? Could it lead to clots? Or, if the drug builds up, could it cause dangerous bleeding? The answer isn’t one-size-fits-all. For most DOACs, the data now shows that standard dosing works fine-even in people with extreme obesity. But one major exception stands out.Apixaban: The Most Reliable Choice
Apixaban, taken twice daily at 5 mg (or 2.5 mg for patients over 80, under 60 kg, or with kidney issues), is the most consistently safe and effective DOAC in obese patients. Studies involving thousands of patients with BMI over 40 show no increase in stroke or clotting events compared to non-obese users. Major guidelines from the International Society on Thrombosis and Haemostasis (ISTH) and the European Heart Rhythm Association (EHRA) strongly support using standard apixaban doses regardless of weight. Real-world data backs this up. In a study of over 2,100 obese patients on DOACs, those taking apixaban had a major bleeding rate of just 2.1% per year-similar to non-obese patients. In another group of 347 patients with BMI over 50, those on standard-dose apixaban had zero thrombotic events. No dose increases needed. No monitoring required.Rivaroxaban: Also Safe, But Watch the Timing
Rivaroxaban works well too. For atrial fibrillation, the standard 20 mg once daily dose (or 15 mg if kidney function is low) is appropriate for obese patients. For treating blood clots, the initial 15 mg twice daily for 21 days, followed by 20 mg once daily, is still the recommended approach. Like apixaban, rivaroxaban shows no increased bleeding risk in obese patients. The ISTH 2021 guidelines explicitly state that standard rivaroxaban dosing is safe for VTE treatment and prevention-even in patients over 120 kg. Real-world data from U.S. healthcare systems found no difference in stroke or bleeding rates between obese and non-obese patients on rivaroxaban.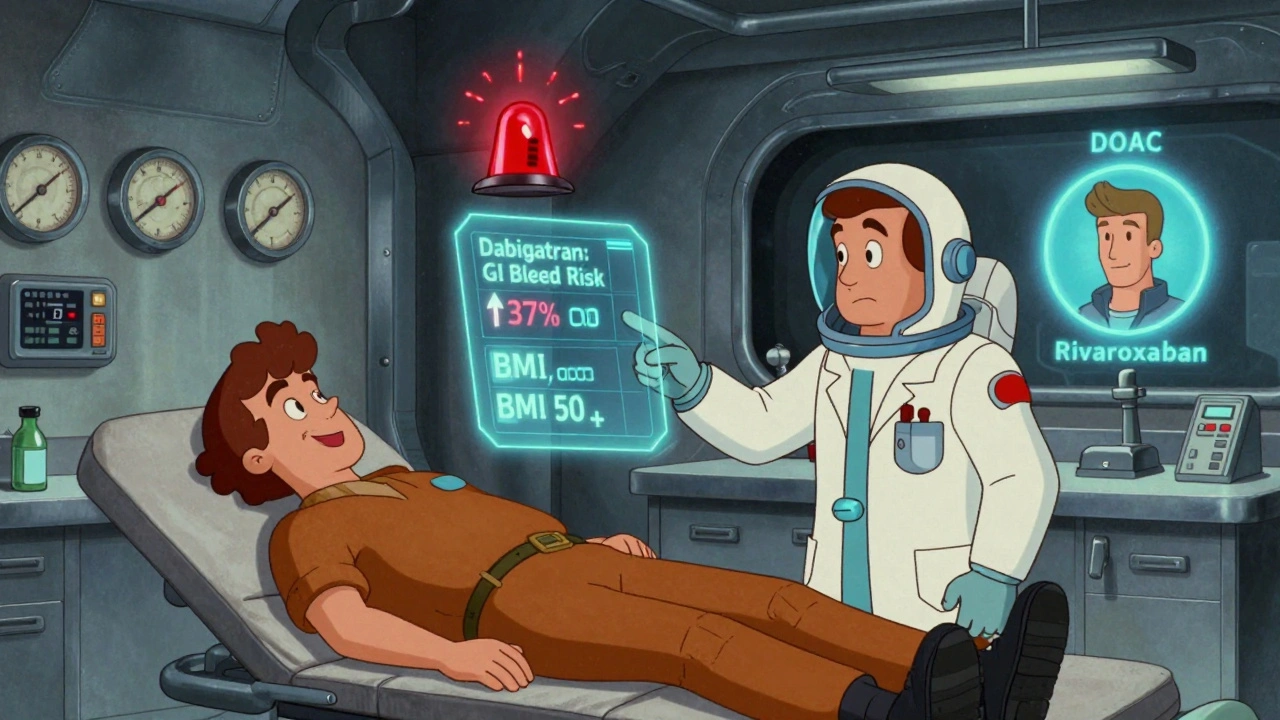
Dabigatran: The One to Avoid in Severe Obesity
Dabigatran is where things get risky. While it works well for preventing strokes in obese patients with atrial fibrillation, it carries a significantly higher risk of gastrointestinal bleeding. Studies show a 37% increase in GI bleeding compared to non-obese patients. For those with BMI over 40, the risk jumps even more-some reports show a 2.3-fold increase in serious GI bleeds. The European Heart Rhythm Association and the Anticoagulation Forum both warn against using dabigatran in morbid obesity. If a patient has a history of ulcers, GERD, or GI bleeding, dabigatran should be avoided entirely. Even in patients without prior GI issues, the data suggests this drug isn’t worth the extra risk when safer options exist.Edoxaban: Mostly Fine, But Watch the Extremes
Edoxaban’s data is more mixed. Standard dosing (60 mg once daily, or 30 mg if kidney function is low or weight under 60 kg) works well for most obese patients. Studies show that anti-Xa levels-the measure of drug activity-stay within therapeutic range across all BMI groups. But here’s the catch: in patients with BMI over 50, some clinicians have seen subtherapeutic levels in nearly 1 in 5 patients on standard-dose edoxaban. That means the drug might not be working well enough. The 2023 ACC/AHA/ACCP/HRS guidelines suggest considering the reduced 30 mg dose in patients with BMI over 50, even if they’re not underweight or kidney-impaired. It’s not a hard rule, but it’s a flag to watch.What About Dose Escalation?
You might think: if standard doses work, why not increase them for bigger patients? The answer is simple: there’s no evidence it helps. In fact, the ISTH 2021 guidelines explicitly say do not increase DOAC doses beyond standard regimens in obese patients. Higher doses don’t lower clot risk-they just raise bleeding risk. One study looked at 150 obese patients given double the standard dose of apixaban. The result? More bleeding, no fewer clots. That’s the danger of guessing. DOACs aren’t like insulin or antibiotics where you adjust based on weight. Their design makes them forgiving-but only if you stick to the approved doses.
Real Numbers, Real Risks
Let’s put this in perspective. In the U.S., over 42% of adults are obese (BMI ≥30), and nearly 10% have morbid obesity (BMI ≥40). That’s millions of people on anticoagulants. Since 2014, DOACs have gone from 32% to 78% of new prescriptions for obese patients with atrial fibrillation. Why? Because the evidence works. Here’s what the numbers show for standard-dose DOACs in obese patients:- Stroke/systemic embolism rate: 1.3-1.4 per 100 patient-years (same as non-obese)
- Major bleeding rate: 2.1-2.4% per year for apixaban and rivaroxaban
- GI bleeding with dabigatran: 37% higher than non-obese patients
- Subtherapeutic levels with edoxaban (BMI >50): up to 18.2%
What Should You Do?
If you or someone you care for has obesity and needs a blood thinner, here’s what to ask:- Is this for atrial fibrillation or a blood clot? (Different dosing rules apply.)
- What’s the BMI or actual weight? (Over 120 kg or BMI >40? That matters.)
- Has there been any history of GI bleeding or ulcers? (Avoid dabigatran if yes.)
- Are kidney function and age being considered? (Apixaban dose drops to 2.5 mg if age ≥80, weight ≤60 kg, and creatinine ≥1.5.)
- Is there a plan to monitor? (Routine testing isn’t needed-but if BMI is over 50, consider checking anti-Xa levels if there’s concern.)
What’s Next?
A major trial called DOAC-Obesity (NCT04588071) is currently enrolling 500 patients with BMI ≥40 to definitively answer dosing questions. Results are expected in late 2024. Until then, the best advice is this: stick to standard doses of apixaban or rivaroxaban. Avoid dabigatran in severe obesity. Use edoxaban cautiously if BMI is over 50. The goal isn’t to overcomplicate treatment. It’s to use the right drug, at the right dose, without guessing. For most obese patients, that’s apixaban or rivaroxaban-safe, effective, and proven.Can I take a higher dose of apixaban if I’m very obese?
No. There is no evidence that increasing the dose of apixaban beyond the standard 5 mg twice daily (or 2.5 mg twice daily for qualifying patients) improves outcomes. Higher doses increase bleeding risk without reducing clot risk. Stick to the approved dosing guidelines.
Is dabigatran ever safe for obese patients?
Dabigatran can be used in patients with mild to moderate obesity (BMI 30-40), but it should be avoided in morbid obesity (BMI ≥40). Studies show a 37% higher risk of gastrointestinal bleeding in obese patients compared to non-obese patients, and a 2.3-fold increase in severe GI bleeds for those with BMI over 40. Safer alternatives like apixaban and rivaroxaban are preferred.
Do I need blood tests to monitor DOACs if I’m obese?
Routine blood tests like INR are not needed for DOACs, even in obese patients. These drugs have predictable effects and don’t require monitoring. However, if BMI is over 50 and there’s concern about effectiveness (e.g., a clot event despite therapy), anti-Xa levels can be checked to confirm therapeutic exposure.
Why are apixaban and rivaroxaban better than warfarin in obese patients?
Warfarin requires frequent blood tests, has many food and drug interactions, and is harder to control in obese patients due to variable metabolism. DOACs like apixaban and rivaroxaban have fixed dosing, no routine monitoring, and consistent results across weight ranges. Studies show they’re just as effective and safer in terms of brain bleeding and overall safety.
What if my weight changes after I start a DOAC?
If you gain or lose a significant amount of weight, talk to your doctor. For most patients, standard DOAC doses remain appropriate. But if weight drops below 60 kg or BMI falls below 18.5, dose adjustments may be needed-especially for edoxaban. If weight increases beyond 160 kg or BMI exceeds 50, consider checking drug levels if there’s concern about effectiveness.



George Graham
December 4, 2025 AT 08:51Apixaban has been a game-changer for my dad-he’s 130 kg and on the 5mg twice daily. No bleeding, no clots, no headaches. Docs used to want to crank it up, but we stuck to guidelines and he’s been fine for 3 years now.
John Filby
December 6, 2025 AT 00:32Just had my first apixaban refill and I’m 140kg. Was nervous AF but the doc said ‘no changes needed’ and honestly? I feel better than I did on warfarin. No more weekly blood draws 😭
Elizabeth Crutchfield
December 6, 2025 AT 16:15why is dabigatran still even an option?? i had a friend bleed out from a GI bleed on it and she was only 110kg. not worth it. apixaban all the way.
Ben Choy
December 8, 2025 AT 08:48Love that this post breaks it down so clearly. I’m a nurse in the UK and we’ve switched almost all obese AF pts to apixaban. Rivaroxaban’s fine too, but dabigatran? We just don’t touch it anymore. Real world data matches the guidelines. 🙌
Emmanuel Peter
December 9, 2025 AT 20:20Wait-so you’re telling me the pharmaceutical companies didn’t test these drugs properly on obese people? Of course they didn’t. They test on skinny college kids and then sell it to everyone. This is capitalism in action. They profit off your ignorance. You think your ‘standard dose’ is safe? It’s just the cheapest dose they could get approved with.
Ashley Elliott
December 10, 2025 AT 22:36Thank you for this. So many people don’t realize that ‘normal’ dosing isn’t one-size-fits-all-and that’s okay. I’ve had patients panic when they hear ‘you’re obese’ like it’s a crime. But the data’s clear: apixaban works. No need to overthink it. Just follow the guidelines. You’re not broken-you’re just human.
Chad Handy
December 11, 2025 AT 03:52I’ve been on rivaroxaban for 4 years. 150kg. No problems. But last month my knee started swelling. I thought it was arthritis. Then I went to the ER and they said ‘your anti-Xa level is subtherapeutic.’ I was pissed. I’ve been taking it exactly as prescribed. Now they’re switching me to apixaban. So… what’s the point of even having a ‘standard dose’ if it doesn’t work for everyone? They’re just guessing. And now I’m stuck paying for another med. This system is broken.
Augusta Barlow
December 12, 2025 AT 20:04Did you know the FDA approved DOACs based on trials where less than 2% of participants had BMI over 40? That’s not science-that’s a marketing ploy. The same people who told us Vioxx was safe are now telling us apixaban is fine. They’re all connected. Big Pharma owns the guidelines. The ISTH? EHRA? All funded by drug companies. They don’t want you to know that edoxaban fails in 18% of obese patients because then people would stop buying it. Wake up.
Joe Lam
December 12, 2025 AT 22:36Apixaban? Really? That’s the best you’ve got? I’ve read the actual trial data-those ‘obese’ participants were defined as BMI 30+, which is just overweight. True morbid obesity? They excluded them. So you’re basing guidelines on data that doesn’t even include the people you’re prescribing to. That’s not medicine. That’s lazy.
Jenny Rogers
December 14, 2025 AT 09:32It is a moral imperative, in the context of contemporary biomedical ethics, to eschew pharmacological empiricism in favor of evidence-based, weight-agnostic dosing paradigms. The conflation of anthropometric metrics with therapeutic efficacy constitutes a form of epistemic injustice, wherein patients are pathologized for their corporeal existence rather than treated as autonomous agents within a scientifically rigorous framework. Apixaban, as the most pharmacokinetically stable agent, represents not merely a clinical preference, but an ethical necessity.
Rachel Bonaparte
December 16, 2025 AT 04:37Okay but what if your doctor is just lazy and doesn’t want to order labs? What if they just say ‘apixaban 5mg’ because it’s easier than thinking? And then you have a clot and they say ‘oh well, you’re obese so it’s probably your fault.’ I’ve seen this happen. The guidelines are great on paper, but in practice? Doctors use them as a shield. They don’t care. They just want to check the box.
Scott van Haastrecht
December 17, 2025 AT 11:28Apixaban is a lie. I know a guy who took it for 2 years, lost 80 pounds, and then had a stroke. They never re-evaluated his dose. They just kept giving him the same 5mg. He’s now in a nursing home. This isn’t medicine-it’s a gamble with your life. And the doctors? They’re too scared to admit they made a mistake.
Chase Brittingham
December 19, 2025 AT 07:40Just wanted to say thanks for this. I’m a 145kg guy with AFib and I was terrified to start anything. I read the whole post, showed it to my doc, and we went with apixaban. No blood tests, no stress. I feel like I finally got good advice instead of being treated like a number. You don’t need to overcomplicate it. Sometimes the simplest answer is the right one.