TB Drug Therapy: What Works, What Doesn't, and How to Stay on Track
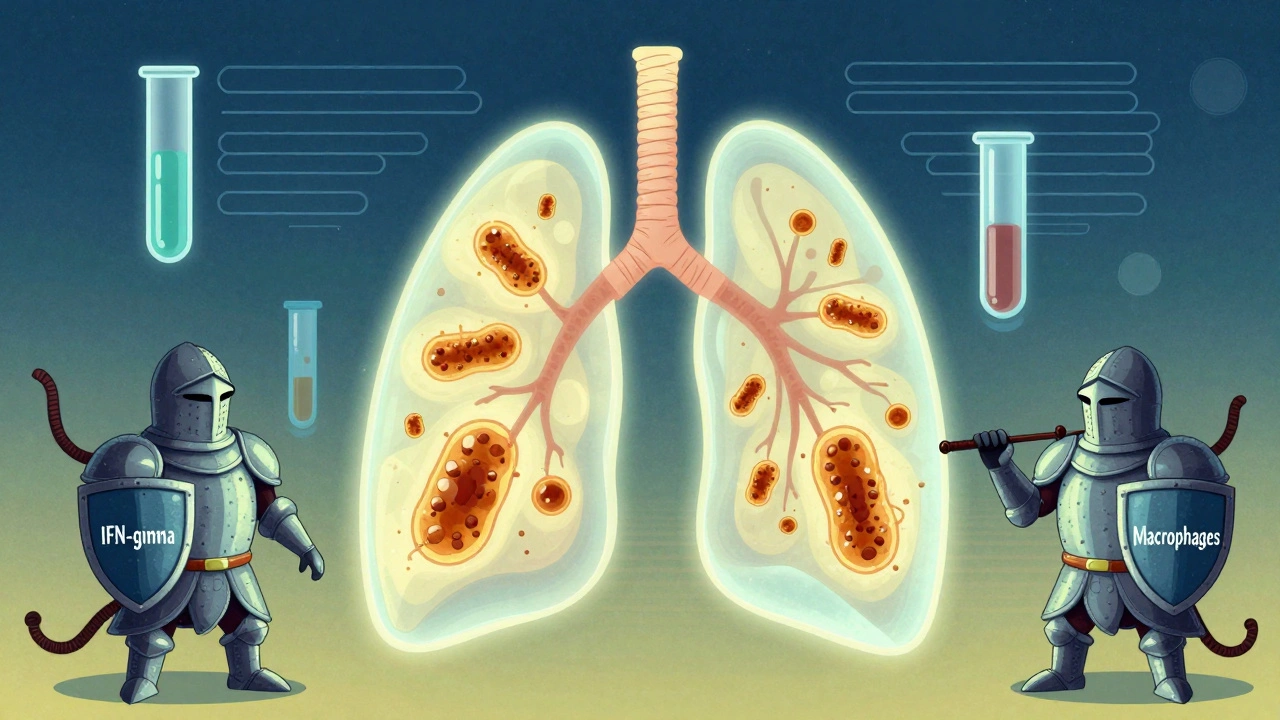
When it comes to TB drug therapy, a multi-drug treatment regimen designed to kill Mycobacterium tuberculosis bacteria over several months. Also known as anti-TB treatment, it’s one of the most time-sensitive, high-stakes drug regimens in modern medicine. Unlike a simple antibiotic for a sore throat, TB drug therapy isn’t a quick fix. It demands strict, daily adherence for at least six months—sometimes longer—because the bacteria hide deep in lung tissue and can wake up if you stop too soon.
This isn’t just about taking pills. It’s about preventing drug-resistant TB, which turns treatable infections into deadly ones. If you skip doses or quit early, the toughest bacteria survive and multiply. That’s how multidrug-resistant TB (MDR-TB) forms, needing 18–24 months of harsher, more expensive drugs with serious side effects. The World Health Organization reports over 400,000 new MDR-TB cases every year, mostly because treatment wasn’t completed correctly. That’s why medication adherence, the consistent, correct use of prescribed drugs over time. Also known as treatment compliance, it’s the single biggest factor in curing TB and stopping its spread. Studies show patients who stick to their regimen have a 95% cure rate. Those who don’t? Their chances drop below 60%.
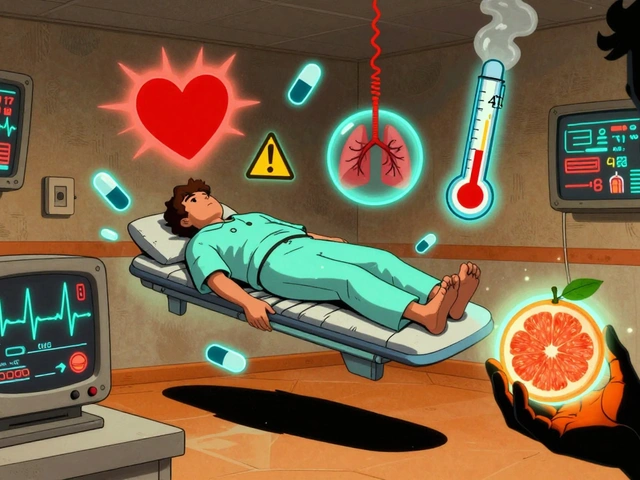
What makes TB drug therapy so tricky? First, the pill burden. Most patients take four drugs at once: isoniazid, rifampin, pyrazinamide, and ethambutol. That’s a handful of pills every day, sometimes with food restrictions or timing rules. Then there are side effects—nausea, liver stress, nerve tingling, even vision changes. Many people think they’re getting better after a few weeks and cut back. But TB bacteria can still be alive, quietly rebuilding. That’s why tracking your progress matters. Keeping a medication journal, a simple log of when you take each drug, how you feel, and any side effects. Also known as treatment diary, it helps you and your doctor spot problems early. It’s not about perfection—it’s about awareness. One patient in a CDC study caught a liver reaction just by noticing yellowing skin in her journal. She got help before it turned dangerous.
And it’s not just about the drugs. TB thrives in crowded, poorly ventilated spaces. It spreads through the air. So even if you’re taking every pill, you need to protect others—especially in the first few weeks. That’s why public health workers often use directly observed therapy (DOT), where a nurse watches you swallow each dose. It sounds strict, but it saves lives. And it’s not just for low-income areas. In the U.S., DOT is standard for patients with history of missed doses, homelessness, or substance use.
What you’ll find below are real stories and science-backed tips from people who’ve been through it. From how to handle nausea without quitting, to why switching generics can affect your response, to what to do when insurance denies your prescription. These aren’t theoretical guides—they’re practical tools for surviving a long, demanding treatment. Whether you’re a patient, a caregiver, or just trying to understand why TB takes so long to cure, this collection gives you what you need to stay on track, avoid resistance, and get well for good.
 1 December 2025
1 December 2025
Tuberculosis: Understanding Latent Infection, Active Disease, and How Drug Therapy Works
Tuberculosis can remain hidden for years as latent infection or become deadly as active disease. Learn how to tell them apart, why treatment differs, and how drug therapy stops transmission and saves lives.
Latest Posts
-
When to Seek Medical Help for a Suspected Drug Interaction
-

Stereospermum Plant Guide: Uses, Health Benefits, and Growing Tips
-

Travel Sickness and the Elderly: Caregiver Tips for a Smooth Journey
-

How to Store Sumatriptan: Tips for Keeping Your Medication Safe and Effective
-

Best CVS Alternatives: Top Pharmacies & Online Prescription Services in 2025

15