Diuretic Hydration: What It Is, How It Works, and What You Need to Know
When you take a diuretic, a medication that increases urine output to remove excess fluid from the body. Also known as water pills, it helps with high blood pressure, heart failure, or swelling—but it doesn't mean you should drink more water blindly. Diuretic hydration isn’t about chugging gallons. It’s about balancing what you lose with what you need to keep your body running right.
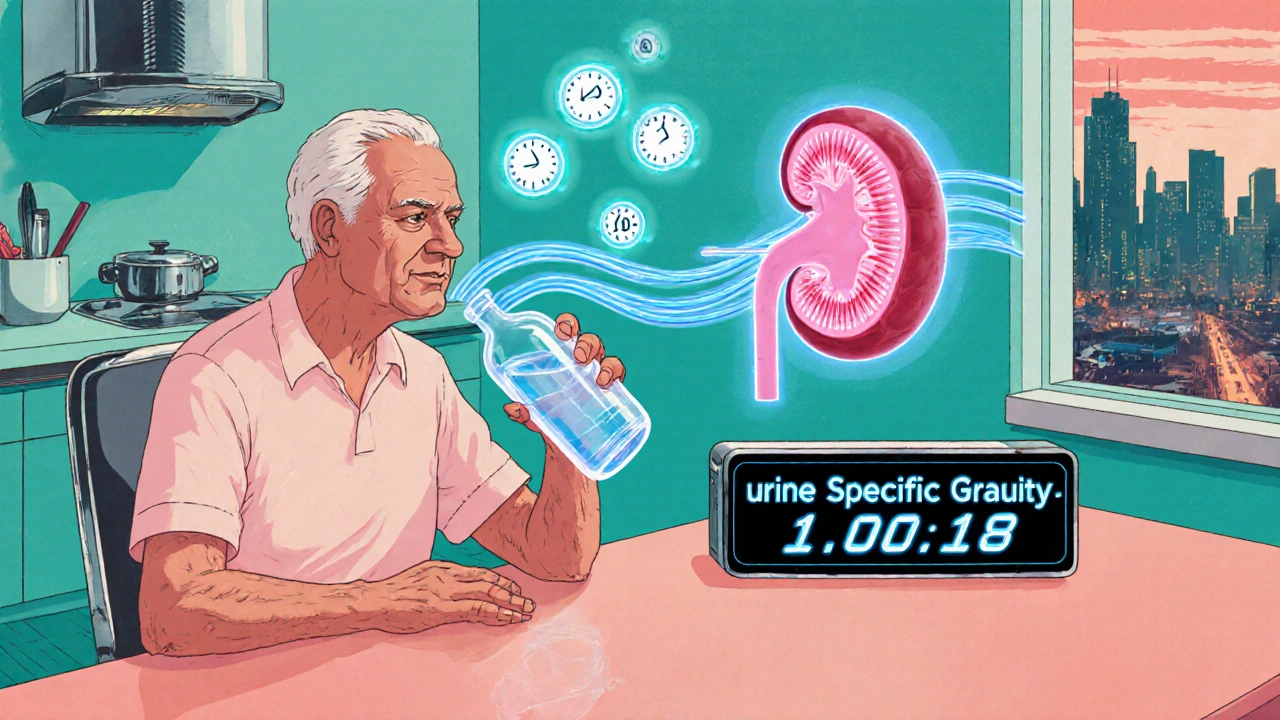
Diuretics work by telling your kidneys to flush out sodium and water. But when sodium leaves, so do other electrolytes like potassium and magnesium. That’s why people on diuretics often feel tired, crampy, or dizzy—not because they’re dehydrated, but because their electrolytes, minerals that control nerve and muscle function, including sodium, potassium, calcium, and magnesium. Also known as mineral salts, they are critical for maintaining fluid balance and heart rhythm. are out of whack. A 2023 study in the Journal of Clinical Hypertension found that nearly 40% of patients on long-term diuretics had low potassium levels, even when they drank enough water. Drinking more won’t fix that. You need to replace what’s lost.
Not all diuretics are the same. Some, like hydrochlorothiazide, make you lose potassium. Others, like spironolactone, help you keep it. Your doctor picks one based on your condition—not just to reduce swelling, but to protect your heart and muscles. If you’re on a diuretic and notice frequent urination, dry mouth, or muscle weakness, it’s not normal thirst. It’s a signal your body is losing more than water. That’s where fluid balance, the body’s system of regulating water intake, output, and distribution to maintain stable internal conditions. Also known as homeostasis of hydration, it’s the key to avoiding both dehydration and dangerous fluid overload. comes in. It’s not just about volume. It’s about quality—what’s in your urine, what’s left in your blood, and whether your kidneys are still working right.
Many people think if they’re peeing a lot, they must be drinking too little. That’s backwards. Diuretics force fluid out, so your body can’t hold onto it the way it used to. If you cut back on water, you risk kidney strain. If you overdo it, you might dilute your blood too much. The sweet spot? Drink when you’re thirsty, eat foods rich in potassium like bananas and spinach, and skip the salty snacks. No need for sports drinks unless you’re sweating hard. Most people on diuretics do fine with plain water and a balanced diet.
What you’ll find in the posts below aren’t generic tips. They’re real, practical insights from people who’ve been there—how to spot early signs of imbalance, why some meds make dehydration worse, how to talk to your doctor about electrolyte tests, and what to do when a diuretic stops working the way it should. This isn’t about guessing. It’s about knowing what your body’s telling you—and how to respond before it turns into a problem.
 28 November 2025
28 November 2025
Elderly Dehydration and Diuretics: How to Protect Kidneys and Prevent Hospitalization
Elderly people on diuretics face a high risk of dehydration and kidney injury. Learn how to recognize early signs, adjust fluid intake, and prevent hospitalization with simple, proven strategies backed by current medical research.
Latest Posts
-

Authorized Generic Pricing: Why They Cost Less Than Brand Name Drugs
-
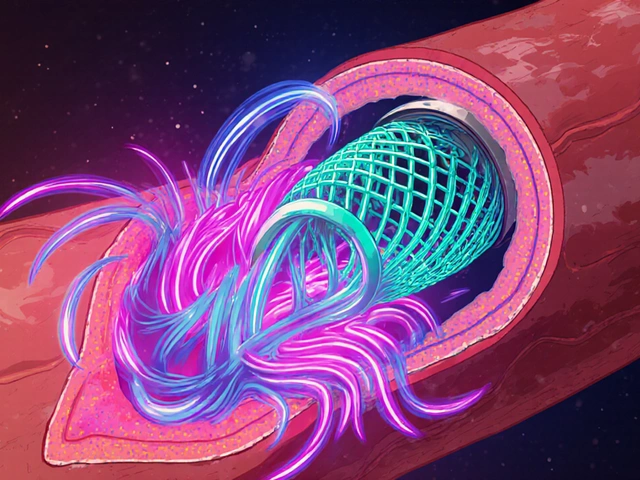
How High Blood Pressure Increases Risk of Blood Clots in Stents
-

How to Buy Cheap Generic Seroquel Online Safely
-

Trazodone vs. Alternatives: Which Sleep Aid Is Right for You?
-

Latisse vs. Alternatives: Which Eyelash Growth Solution Is Right for You?

11