Atrophic gastroenteritis: what it is and why it matters
Atrophic gastroenteritis (also called atrophic gastritis) means the stomach lining has thinned and lost some of its normal function. That thin lining makes less acid and fewer enzymes, so digestion changes and vitamin B12 absorption can fall. Over time this can cause anemia, nerve symptoms, and higher risk of certain stomach problems.
This condition often develops slowly. You might not notice anything at first, or you could have long-standing indigestion that never fully goes away. The key is spotting warning signs early and treating the cause when possible.
Common causes and typical symptoms
Two main causes come up a lot: chronic Helicobacter pylori infection and autoimmune attack on the stomach lining. H. pylori is a bacteria many people carry for years. Autoimmune atrophic gastritis happens when the immune system targets stomach cells and the intrinsic factor that helps absorb B12.
Symptoms vary. Some people have bloating, mild upper belly pain, nausea, poor appetite, or unintentional weight loss. Other signs point to low B12 or iron—fatigue, pale skin, shortness of breath, tingling or numbness in hands and feet, or trouble concentrating. Because symptoms overlap with other stomach problems, tests usually decide the diagnosis.
How doctors diagnose and treat it
Diagnosis usually involves an upper endoscopy with biopsies so the doctor can see thinning and check for H. pylori. Blood tests look for low B12 or iron, a complete blood count, and sometimes antibodies against intrinsic factor. Breath or stool tests help find H. pylori without endoscopy.
Treatment focuses on what’s causing the damage and on replacing missing nutrients. If H. pylori is present, antibiotics plus acid-reducing medicine can often clear the infection and stop further harm. If B12 is low, doctors give injections or high-dose oral B12 depending on the situation. Iron supplements may be needed if iron deficiency is found. People with autoimmune atrophic gastritis need ongoing monitoring because their stomach acid and intrinsic factor may remain low.
In cases with advanced atrophy, your doctor may recommend periodic follow-up endoscopies to check for precancerous changes. That doesn’t mean cancer is certain, but monitoring catches problems early.
Everyday tips that help
Small, regular meals that are easy to digest usually feel better than large heavy meals. Cut back on alcohol, tobacco, and NSAIDs (ibuprofen, naproxen) which can irritate the stomach. Avoid very spicy or greasy foods if they bother you. Talk to your doctor before starting supplements—B12 is commonly needed, while probiotics or digestive enzymes can help some people but aren’t a replacement for medical care.
If you have persistent indigestion, symptoms of anemia, or new neurologic symptoms like numbness, see your doctor. With the right tests, treatment, and follow-up, most people manage symptoms well and lower future risks. Keep track of changes, ask for B12 checks if you feel tired or numb, and work with your clinician on a clear plan.
 21 July 2023
21 July 2023
The Importance of Regular Checkups for Atrophic Gastroenteritis Patients
In my recent blog, I highlighted the crucial role of regular check-ups for those suffering from Atrophic Gastroenteritis. It's vital to understand that consistent monitoring can help manage this condition effectively by detecting any changes early. Regular check-ups also help in adjusting treatment plans if needed, ensuring that patients continue to live a quality life. With atrophic gastritis being a chronic condition, it's essential to stay on top of it to prevent it from worsening. So, don't skip those appointments, as they are instrumental in your journey towards health.
Latest Posts
-

Cialis Super Active vs Alternatives: What Works Best for ED?
-
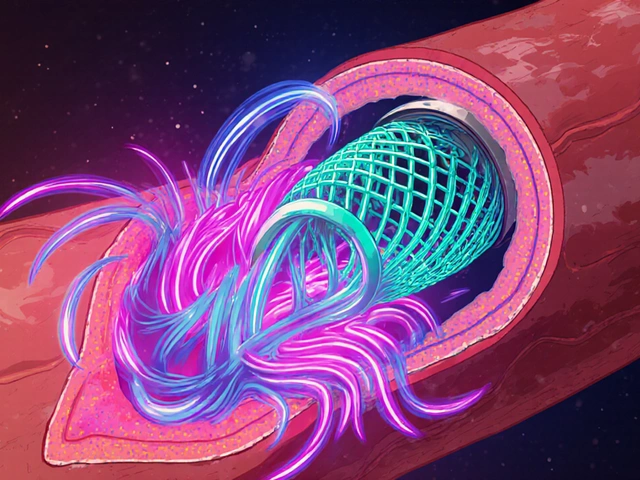
How High Blood Pressure Increases Risk of Blood Clots in Stents
-

Pituitary Adenomas: Understanding Prolactinomas and Hormone Imbalances
-

Understanding Bladder Pain and Pelvic Floor Dysfunction: Key Insights
-

European Generic Markets: Regulatory Approaches Across the EU in 2025

5