Specialty medications and injectables are saving lives-but they’re also breaking budgets. These drugs treat serious conditions like cancer, rheumatoid arthritis, multiple sclerosis, and hepatitis C. But they don’t come cheap. Many cost over $1,000 a month. Some even hit $20,000. And they’re not going away. In fact, they’re growing faster than any other part of the pharmacy market. In 2023, specialty drugs made up just 2% of all prescriptions but consumed half of all pharmacy spending. If you’re paying for these meds-whether through an employer plan, Medicare, or out of pocket-you’re feeling the pinch.
Know What You’re Paying For
Before you can save money, you need to understand what you’re spending on. Specialty medications aren’t like your usual pills. They often require special storage, trained staff to administer them, and frequent monitoring. That’s why they’re priced so high. But not all of that cost is justified. Some of it comes from lack of competition, complex distribution chains, and opaque pricing.Ask your doctor or pharmacist: Is this drug truly necessary? Is there a generic or biosimilar version? Could it be given at home instead of in a hospital? These simple questions can open the door to big savings.
Switch to Biosimilars When Possible
Biosimilars are the closest thing to generic versions of biologic drugs. They’re not exact copies-biologics are too complex for that-but they work the same way, with the same safety and effectiveness. And they cost about half as much.As of 2023, the FDA had approved 42 biosimilars. Yet adoption is still under 30% in most therapeutic areas. Why? Many doctors aren’t familiar with them. Patients are wary. Insurance plans don’t always push them.
But the savings are real. For example, a biosimilar version of Humira (adalimumab) can cut monthly costs from $2,500 to $1,200. Over a year, that’s $15,600 saved. Hospitals and clinics that switched to biosimilars saw 20-30% reductions in drug spend-without any drop in patient outcomes.
Don’t assume your current drug is the only option. Ask your doctor: “Is there a biosimilar available for this medication?” If they say no, ask why. Often, it’s just habit-not medical necessity.
Use a Narrow Pharmacy Network
Not all pharmacies are created equal. Specialty medications are often distributed through a small group of high-cost specialty pharmacies. But some insurers have partnered with a limited number of these pharmacies to get better pricing.These “narrow networks” can cut costs by 10-15%. How? Because they negotiate bulk discounts, provide better patient support, and reduce administrative waste. Employers using these networks saved $1.37 per member per month-$35 million a year across 200 companies.
If your plan offers a preferred specialty pharmacy, use it. You might need to switch from your local pharmacy, but the savings can be huge. And you’ll likely get better service: dedicated nurses, medication delivery, refill reminders, and help with insurance paperwork.
Some people resist switching because they’re used to their current pharmacy. But the trade-off is worth it. One study found patients using preferred networks rated their support services 8.7 out of 10-compared to 7.2 for non-preferred ones.
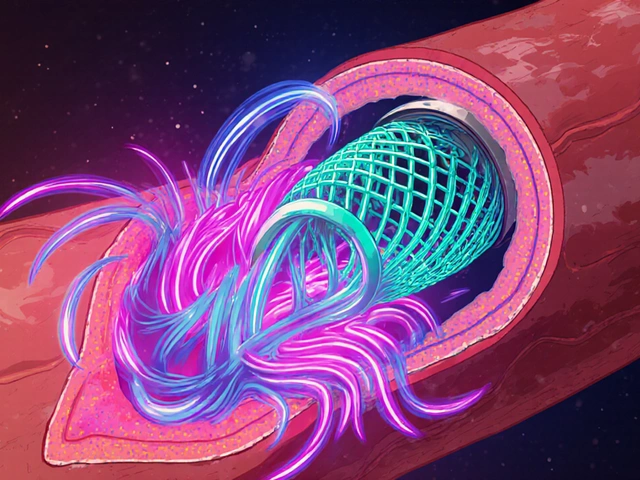
Move Administration to Lower-Cost Settings
Many injectables are given in hospital outpatient departments-even when they don’t need to be. Why? Tradition. Convenience. Lack of awareness.But giving the same shot in a doctor’s office, clinic, or even at home can slash costs by 40-50%. A single infusion that costs $1,200 in a hospital might cost just $600 in a clinic. For patients getting monthly treatments, that’s $7,200 saved a year.
There are over 220 specialty drugs where hospital administration isn’t medically required. In fact, 91% of cases can safely move to lower-cost settings. The key is coordination. Your doctor needs to approve it. Your insurer needs to cover it. And you need to know your options.
Ask: “Can this injection be given at my doctor’s office or even at home?” If yes, push for it. Many patients don’t know this is even an option.
Use Prior Authorization Wisely
Prior authorization is when your insurer requires approval before covering a drug. Many people see it as a hassle. But done right, it saves money without hurting care.For example, one insurer used prior authorization to limit unnecessary use of GLP-1 weight loss drugs. They saved $13.64 per member per month-without blocking patients who truly needed them. And 87% of employers using this approach said it worked well.
But there’s a catch: if prior authorization is too strict, patients delay or skip treatment. That leads to worse outcomes-and higher costs down the line.
Look for plans that use evidence-based criteria, not just cost-cutting rules. Ask your insurer: “What clinical guidelines do you use to approve these drugs?” If they can’t answer, it’s a red flag.
Get Help with Financial Assistance
Drug manufacturers often offer copay assistance programs. These can reduce your out-of-pocket cost to $0. But here’s the trick: some plans count that assistance toward your deductible. That means you pay more later.That’s where “copay maximizers” come in. These are programs that ensure manufacturer assistance doesn’t count toward your deductible. So you pay $0 now-and your deductible stays intact for other medical costs.
Not all insurers offer this. But many do. Ask your pharmacy or plan: “Do you have a copay maximizer program for this drug?” If not, ask why. It’s a simple fix that can make a huge difference.
Push for Value-Based Contracts
Traditional drug pricing means you pay the same whether the drug works or not. Value-based contracts change that. The drug maker agrees to refund money if the drug doesn’t work as expected.For example, a cancer drug might come with a guarantee: if the tumor doesn’t shrink after three months, you get part of your money back. These deals are rare-but growing. In 2023, value-based arrangements for specialty drugs jumped 45% from the year before.
If you’re part of a large employer or health plan, ask: “Are we using any value-based contracts for our specialty drugs?” If not, suggest it. It’s the most fair way to pay for expensive meds: only pay for results.

Watch for Policy Changes
The government is starting to act. The Inflation Reduction Act lets Medicare negotiate drug prices for the first time. And in 2023, CMS announced it would start paying the same amount for biologics and their biosimilars-ending the old system where biosimilars got paid less, even though they cost less.This change alone could save billions. It’s also pushing private insurers to follow suit. Keep an eye on your plan’s communications. Changes in reimbursement rules often lead to lower prices for patients.
What You Can Do Right Now
You don’t need to wait for your employer or insurer to fix things. Here’s your action list:- Ask your doctor: “Is there a biosimilar version of this drug?”
- Ask your pharmacy: “Are we using a preferred specialty pharmacy?”
- Ask your insurer: “Can this injection be given at home or in a clinic instead of a hospital?”
- Ask your plan: “Do you have a copay maximizer program?”
- Check if your drug is covered under a value-based contract.
These five questions can save you thousands. And they take less than 10 minutes to ask.
Don’t Accept High Costs as Normal
Specialty drugs are expensive-but they don’t have to be this expensive. The system is built to profit, not to protect patients. But you have power. You can ask for better options. You can demand transparency. You can choose lower-cost alternatives.Every time you speak up, you help not just yourself-but others too. Because when one person finds a way to save, it pushes the whole system to change.
Are biosimilars safe to use instead of brand-name biologics?
Yes. Biosimilars are approved by the FDA after rigorous testing to prove they work the same as the original biologic drug. They have the same active ingredients, dosage, and safety profile. Over 40 biosimilars are on the market, and studies show no difference in effectiveness or side effects. Many patients switch without any issues.
Why do some doctors refuse to prescribe biosimilars?
Some doctors are unfamiliar with biosimilars or worry patients will be confused. Others are influenced by drug reps or outdated guidelines. But this is changing. As more data shows biosimilars work just as well, and as patients ask for them, doctors are becoming more open. If your doctor says no, ask for the reason-and suggest you both look up the latest FDA and clinical guidelines together.
Can I get specialty medications delivered to my home?
Yes, many specialty medications can be delivered directly to your home. This is especially common for injectables and infusions. Home delivery often comes with clinical support: nurses who train you on self-administration, refrigeration supplies, and 24/7 helplines. It’s safer, more convenient, and usually cheaper than picking up at a pharmacy or going to a hospital.
Why is my insurance denying coverage for my specialty drug?
Denials usually happen because the drug isn’t on your plan’s formulary, or because prior authorization wasn’t completed. Sometimes, the insurer thinks a cheaper alternative exists. Don’t take a denial as final. Ask for the reason in writing, then appeal. Most denials are overturned on appeal, especially if your doctor provides clinical documentation showing why the drug is necessary.
How do I find out if my plan has a preferred specialty pharmacy?
Check your insurance plan’s website under “Specialty Pharmacy” or “Drug Coverage.” You can also call the member services number on your card and ask: “Which specialty pharmacies are in-network for my plan?” If you’re currently using a non-preferred pharmacy, ask if you can switch. Many plans will help you transfer your prescriptions with no disruption.
Will switching to a lower-cost setting affect the quality of my care?
No. Studies show that care quality stays the same-or even improves-when specialty injections move from hospitals to clinics or home settings. In fact, patients often get better support at home: personalized training, fewer delays, and less exposure to germs. The only difference is the location-and the cost.
Next Steps
If you’re paying for specialty meds, don’t wait for someone else to fix it. Start with one step today: call your pharmacy or insurer and ask if there’s a biosimilar or lower-cost administration option for your drug. Write down the answer. Then ask again next month. Progress happens one question at a time.Specialty drugs aren’t going away. But their prices can be brought down-if patients, doctors, and plans work together. You’re not powerless. You’re part of the solution.




Gerald Tardif
December 28, 2025 AT 20:30Been there. My wife’s on a biosimilar for RA now-cut our monthly bill from $2,800 to $1,300. No side effects, no drama. Just cheaper magic.
Doctors don’t always push it, but if you ask, they’ll admit they’ve seen it work.
It’s not about cutting corners-it’s about cutting waste.
Monika Naumann
December 29, 2025 AT 07:18It is a disgrace that Western nations allow such pharmaceutical exploitation to occur. In India, we have long understood that medicine must serve humanity-not corporate shareholders. The arrogance of American pricing is not just unethical-it is a moral failure of civilization.
Anna Weitz
December 30, 2025 AT 06:16They don’t want you to know this but biosimilars are just rebranded generics with a fancy label and a higher profit margin for Big Pharma
They’re not safer they’re just cheaper to make and the FDA lets them slide because they’re too cozy with the labs
And don’t get me started on home delivery-what’s next telepathic insulin?
It’s all a scam to make you think you’re saving when you’re just being manipulated
Jane Lucas
December 31, 2025 AT 10:12my doc just shrugged when i asked about biosimilars
i asked again two weeks later and he said oh yeah there is one
we switched and i saved like 60%
he didn’t even mention it first
why is that
Elizabeth Alvarez
January 1, 2026 AT 18:19They’re lying about the savings. The real reason they push biosimilars is because the government is forcing insurers to cut costs-so they’re pushing patients into cheaper drugs that aren’t tested long-term
And home delivery? That’s just the first step to removing all medical oversight
Next thing you know, people are injecting themselves with unregulated stuff from Amazon
And the pharmacies? They’re data miners. They track your health, sell it, then raise your premiums
This isn’t healthcare-it’s a surveillance pipeline disguised as compassion
Miriam Piro
January 2, 2026 AT 03:21Let’s be real-this whole system is rigged. Biosimilars? Sure they’re ‘approved’… but who approved them? The same people who got paid by the big pharma lobbyists
And ‘narrow networks’? That’s just a fancy word for ‘we’re forcing you into one pharmacy that pays us kickbacks’
And value-based contracts? LOL
They’ll refund you if the drug doesn’t work… after you’ve already paid $10K out of pocket
And Medicare negotiating prices? Please. They’ll negotiate… right after they approve the next $50K drug
Wake up people. This isn’t reform. It’s rebranding.
And if you think you’re saving-you’re just being slowly bled dry with a smile on their face 😔
Kylie Robson
January 3, 2026 AT 08:26From a pharmacoeconomic standpoint, the cost containment levers outlined-biosimilar adoption, narrow pharmacy networks, and site-of-service optimization-are all empirically validated interventions with demonstrated ICERs below $50K/QALY
However, the implementation is hampered by provider inertia, payer misalignment, and patient behavioral economics-specifically loss aversion toward perceived brand superiority
The copay maximizer mechanism is particularly underutilized due to structural misalignment between PBMs and plan sponsors-this requires contractual renegotiation to achieve true cost neutrality
Andrew Gurung
January 4, 2026 AT 19:19Wow. So you’re telling me… we can just… *ask* for cheaper options?
Like… a normal person?
Not some corporate drone with a clipboard?
Are you kidding me?
I’ve been paying $2,500/month for 3 years thinking I had no choice.
Turns out… I just needed to open my mouth.
My therapist says I have ‘medical trauma’ now.
Thanks, internet.
😭
Will Neitzer
January 5, 2026 AT 04:31This is one of the most practical, compassionate, and well-researched pieces I’ve read on specialty drug pricing in years.
Thank you for not just listing solutions-but explaining *why* they work, and *how* to navigate the system without being overwhelmed.
Many patients feel powerless. You’ve given them a toolkit.
And to those who say ‘it’s too complicated’-it’s only complicated because the system was designed to be.
You’ve cut through the noise.
Well done.
Janice Holmes
January 5, 2026 AT 12:56Okay but let’s be real-why is no one talking about the fact that the FDA approves biosimilars based on *statistical equivalence*, not *biological identity*?
And the ‘narrow networks’? Those are just corporate monopolies with a ‘preferred’ sticker.
And home delivery? That’s how they start tracking your biometrics and selling your data to insurers.
This isn’t saving money-it’s surrendering autonomy.
And don’t even get me started on ‘value-based contracts’-that’s just a fancy way to say ‘we’ll pay you back if you don’t die too soon’
It’s all smoke and mirrors. And I’m tired of being the guinea pig.
Olivia Goolsby
January 6, 2026 AT 03:01Everything you’ve said is a lie… or at least, it’s a half-truth carefully crafted by the pharmaceutical-industrial complex to pacify the masses.
First-biosimilars are NOT equivalent. The FDA only requires ‘similar’-not ‘identical’-and we’ve seen real-world cases of immunogenicity spikes.
Second-narrow networks? That’s how they funnel you to pharmacies owned by the same parent company as your insurer.
Third-home administration? That’s how they cut nurses and shift liability onto patients.
Fourth-copay maximizers? Those are designed to inflate your deductible so you pay more later.
Fifth-value-based contracts? They’re only offered for drugs that are *already* failing in clinical trials.
And Medicare negotiating prices? That’s a PR stunt. The real deals are hidden behind NDAs.
This isn’t reform. It’s psychological manipulation.
And if you believe any of this-you’re part of the problem.
Alex Lopez
January 6, 2026 AT 05:59Look. I’ve worked in pharmacy benefit management for 12 years.
Most of this is legit.
Biosimilars? Solid. Site-of-service savings? Real. Copay maximizers? Underrated gold.
But here’s the kicker: none of this works if your doctor doesn’t know about it.
So yes-ask.
And if they brush you off? Bring printouts.
And if they still say no? Ask for a second opinion.
And if they get defensive? That’s when you know you’re onto something.
It’s not conspiracy. It’s just… lazy.
And you? You’re the antidote.
👍
Robyn Hays
January 6, 2026 AT 14:49When I first asked about biosimilars, my doctor looked at me like I’d asked if I could replace my heart with a toaster.
But I didn’t give up.
I printed out FDA guidelines. I brought a list of 5 other patients who’d switched successfully.
He finally agreed.
Now I pay half.
And guess what? I still feel fine.
Turns out, being informed doesn’t make you a troublemaker.
It makes you your own best advocate.
And that’s not scary.
It’s powerful.
Liz Tanner
January 7, 2026 AT 14:52i switched to the preferred pharmacy last year
they mailed me my meds, called to check in, helped me fill out the paperwork
and i saved $1800 in 6 months
my old pharmacy never even asked if i needed help
why do we still use the ones that treat us like a number?
just asking
Babe Addict
January 9, 2026 AT 07:25Everyone’s acting like this is some revolutionary insight but biosimilars have been around since 2015 and we’ve had home delivery since 2010
the real issue is that the system rewards inertia
and patients are too tired to fight
so they keep paying $20K/month because it’s easier than reading a 12-page insurance PDF
it’s not the drugs that are expensive
it’s the apathy