SSRI-NSAID GI Bleeding Risk Calculator
Based on 2022 research showing a 75% increased risk of upper GI bleeding when combining SSRIs and NSAIDs, this calculator helps you understand your personalized risk level.
Recommended Action:
It's generally safe to continue both medications under medical supervision. Consider using a proton pump inhibitor (PPI) like omeprazole for added protection.
Key risk factors:
- Age: Under 65
- SSRI: Sertraline
- NSAID: Celecoxib
When you’re taking an SSRI for depression or anxiety, and you also need pain relief for arthritis or a bad back, it’s easy to reach for an over-the-counter NSAID like ibuprofen or naproxen. But here’s something most people don’t know: combining SSRIs with NSAIDs can double your risk of serious stomach bleeding. This isn’t a rare side effect. It’s a well-documented, preventable danger that affects thousands of people every year - often without either the patient or the doctor realizing it’s happening.
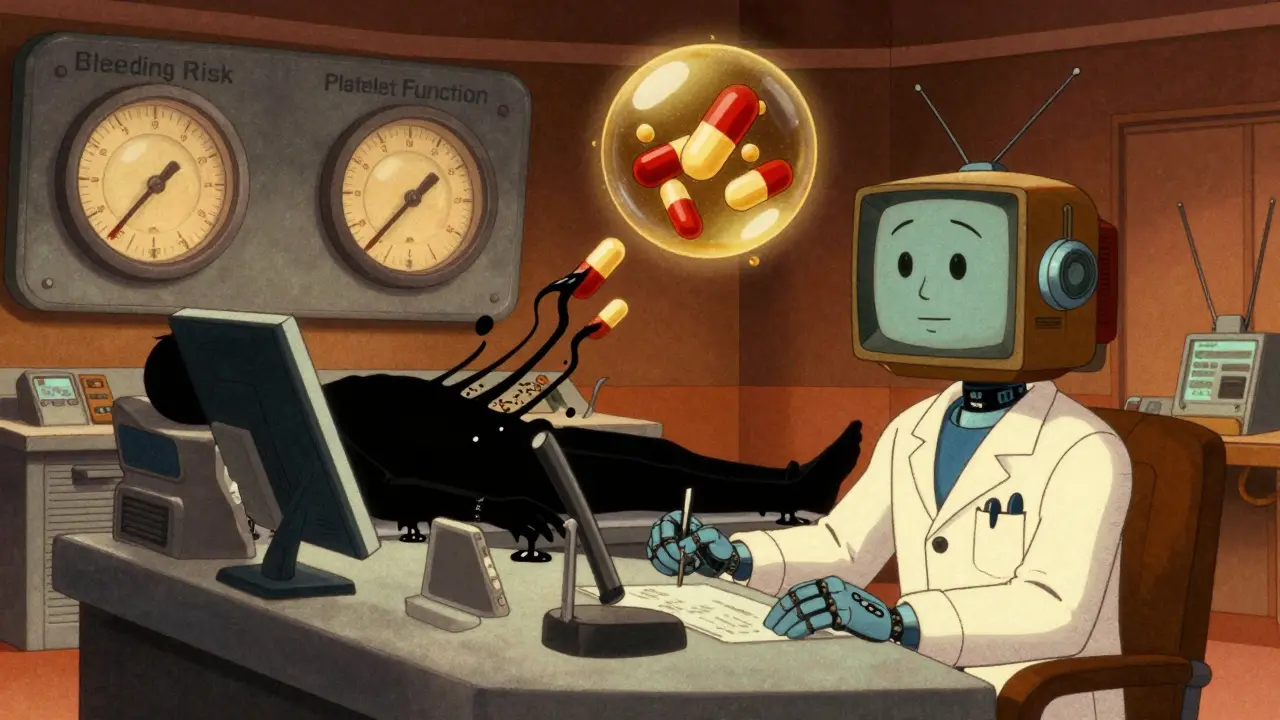
Why This Combination Is So Dangerous
SSRIs like sertraline, fluoxetine, and escitalopram work by boosting serotonin in the brain. But serotonin isn’t just a mood chemical. It’s also critical for blood clotting. Platelets, the cells that stop bleeding, rely on serotonin to stick together and form clots. SSRIs block the serotonin transporter on platelets, which means they can’t grab enough serotonin to do their job properly. This makes platelets less effective at sealing small cuts or scrapes in the stomach lining. NSAIDs like ibuprofen, naproxen, and diclofenac do something else entirely. They shut down enzymes in the stomach that make protective mucus and reduce acid production. Without that mucus shield, the stomach lining becomes vulnerable to damage from its own acid. Over time, this can lead to ulcers. Put them together? You’ve got a one-two punch: your blood can’t clot well, and your stomach lining is already damaged. The result? A much higher chance of internal bleeding - sometimes sudden, sometimes slow, but always dangerous. A 2022 meta-analysis in Nature Scientific Reports that looked at over 1.2 million patients found that people taking both an SSRI and an NSAID had a 75% higher risk of upper GI bleeding than those taking NSAIDs alone. That’s not a small increase. That’s the same risk level as being on blood thinners like warfarin.Who’s Most at Risk?
Not everyone who takes this combo will bleed. But some people are far more vulnerable:- People over 65 - stomach lining thins with age, and platelets don’t work as well.
- Those with a history of ulcers or GI bleeding - if you’ve had one before, you’re far more likely to have another.
- People on multiple medications - adding low-dose aspirin, corticosteroids, or anticoagulants multiplies the risk even further. One study showed the combination of SSRI + NSAID + aspirin raised bleeding risk by more than 12 times compared to no drugs at all.
- High-dose or long-term NSAID users - taking more than 1,200 mg of ibuprofen per day, or using NSAIDs for more than 90 days, significantly increases danger.
Not All SSRIs or NSAIDs Are Equal
The risk isn’t the same across all drugs in these classes. Among SSRIs, drugs like paroxetine and fluoxetine have stronger effects on platelet serotonin uptake, so they may carry slightly higher bleeding risk than sertraline or citalopram. But the difference isn’t big enough to rely on - if you’re on any SSRI and an NSAID, you’re at risk. For NSAIDs, the type matters a lot:- Celecoxib (Celebrex) - a COX-2 inhibitor - has the lowest GI bleeding risk among NSAIDs. It’s still not risk-free, but it’s safer than naproxen or diclofenac.
- Ibuprofen - moderate risk, especially at high doses.
- Naproxen and diclofenac - highest risk. Avoid if possible.

What You Can Do: Prevention Strategies That Work
The good news? This risk is almost entirely preventable. Here’s what actually works, based on guidelines from the American Gastroenterological Association and real-world outcomes:1. Stop the NSAID - If You Can
Before you add an SSRI, ask: Do I really need this NSAID? For many people, especially those with mild to moderate pain, there are safer alternatives.- Acetaminophen (paracetamol) - no interaction with SSRIs. No increased bleeding risk. It’s not as strong for inflammation, but it’s perfect for headaches, muscle aches, and joint pain.
- Physical therapy - for chronic back or knee pain, exercise and movement are more effective long-term than pills.
- Topical NSAIDs - gels or patches like diclofenac gel applied to the skin deliver the drug locally, with almost no systemic absorption. That means minimal stomach risk.
2. If You Must Use Both, Use a PPI
If your pain is severe enough that you need an NSAID, and your depression requires an SSRI, then you need a proton pump inhibitor (PPI) - like omeprazole, esomeprazole, or pantoprazole. PPIs reduce stomach acid, which lets the damaged lining heal. The 2017 Lancet study showed that adding a daily PPI reduces the bleeding risk by 70% in people taking both drugs. That means your risk drops from about 1.5% per year to 0.5% - close to normal. Don’t wait until you’re bleeding to start one. Start the PPI at the same time as the SSRI. It’s not optional - it’s essential.3. Avoid Aspirin Unless It’s Absolutely Necessary
If you’re on an SSRI and an NSAID, adding low-dose aspirin (even 81 mg) is like pouring gasoline on a fire. The JAMA study showed this triple combo raises bleeding risk over 12-fold. If you’re on aspirin for heart protection, talk to your doctor about alternatives - maybe clopidogrel or a different strategy. Don’t assume aspirin is safe just because it’s low-dose.What Patients Are Saying - And Why It Matters
Patient forums are full of stories that sound like warnings from the front lines:- “I was on sertraline and ibuprofen for six months. One morning, I threw up blood. ER visit. Two units of blood. No one told me this could happen.” - MidwestMom, Drugs.com
- “My doctor prescribed fluoxetine and didn’t ask about my naproxen. I ended up in the hospital. I’m lucky I didn’t die.” - Reddit user, r/antidepressants
What Doctors Are Doing About It
Hospitals and clinics are finally catching up:- EHR alerts - electronic health records now flag SSRI-NSAID combos in real time. One study showed this cut bleeding events by 32%.
- GI-BLEED risk calculator - a new tool built into Epic EHR systems uses 12 factors (age, drug types, kidney function, genetic markers) to give each patient a personalized bleeding risk score. It’s 89% accurate.
- Prescription trends - between 2018 and 2022, prescriptions for acetaminophen rose 18% among SSRI users, while NSAID prescriptions dropped 12%. People are switching.
What to Do Right Now
If you’re taking an SSRI and an NSAID, here’s your action plan:- Check your meds. Look at your pill bottles. Do you have both? Write them down.
- Ask your doctor: “Is it safe to take these together? Could my pain be managed without NSAIDs?”
- Ask about PPIs: “Should I be on omeprazole or another stomach protector?”
- Watch for warning signs: Black, tarry stools; vomiting blood or material that looks like coffee grounds; sudden dizziness or weakness; unexplained fatigue. These aren’t normal. Go to the ER.
- Consider alternatives: Acetaminophen, heat packs, physical therapy, or topical gels.
The Bigger Picture
This isn’t just about one drug combo. It’s about how we think about medication safety. We assume OTC drugs are harmless. We assume antidepressants only affect mood. But biology doesn’t work in silos. Serotonin affects your brain, your gut, and your blood. Painkillers don’t just target your knee - they affect your stomach lining. The cost of ignoring this? Over $1.2 billion a year in U.S. healthcare spending - mostly from hospitalizations and emergency visits. And behind every dollar is a person who bled because no one told them this risk existed. The future is changing. New antidepressants like vortioxetine show promise with lower bleeding risk. Pharmacogenomic testing may soon tell us who’s genetically prone to poor drug metabolism. But until then, the solution is simple: know the risk, ask the question, and don’t accept “it’s just ibuprofen” as an answer.Frequently Asked Questions
Can I take ibuprofen with sertraline?
Taking ibuprofen with sertraline increases your risk of stomach bleeding. While the risk is lower than with naproxen or diclofenac, it’s still significant - especially if you’re over 65 or have a history of ulcers. If you need pain relief, acetaminophen is safer. If you must take ibuprofen, use the lowest dose for the shortest time, and always take a proton pump inhibitor like omeprazole at the same time.
Is it safe to take SSRIs with Tylenol (acetaminophen)?
Yes. Acetaminophen (Tylenol) does not interfere with platelet function or damage the stomach lining, so it has no known interaction with SSRIs that increases bleeding risk. It’s the preferred pain reliever for people taking antidepressants like sertraline, fluoxetine, or escitalopram. Just don’t exceed 3,000 mg per day to avoid liver damage.
How long after starting an SSRI does bleeding risk increase?
The risk starts as soon as you begin taking the SSRI - even within the first week. Platelets are affected immediately because they can’t take up serotonin anymore. The longer you’re on both drugs, the higher your cumulative risk. That’s why prevention needs to start on day one, not after you’ve had symptoms.
Do all SSRIs carry the same bleeding risk?
No, but the differences are small. Paroxetine and fluoxetine have stronger effects on platelet serotonin uptake, so they may pose slightly higher risk than sertraline or citalopram. But no SSRI is completely safe when combined with an NSAID. Don’t rely on choosing a “safer” SSRI - focus on avoiding NSAIDs or using a PPI.
Should I stop my SSRI if I need an NSAID?
Never stop an SSRI abruptly. That can cause withdrawal symptoms or make depression worse. Instead, talk to your doctor about alternatives: switch your painkiller to acetaminophen, use a topical NSAID, or start a PPI. If your depression is stable and your pain is mild, you might be able to pause the SSRI temporarily - but only under medical supervision.
What if I’m already bleeding? Should I stop the drugs?
If you’re vomiting blood, passing black stools, or feeling faint, go to the emergency room immediately. Do not wait. At the hospital, they’ll stop the NSAID and likely hold the SSRI until the bleeding is controlled. You’ll need endoscopy, fluids, and possibly a blood transfusion. Afterward, your doctor will help you rebuild your treatment plan with safer alternatives.





Jocelyn Lachapelle
December 16, 2025 AT 17:01I never knew SSRIs and ibuprofen could do this. My mom took both for years and never said a word. So glad I found this. Life-saving info.
Sharing this with everyone I know.
Sai Nguyen
December 18, 2025 AT 16:00Americans think OTC means harmless. That's why your hospitals are full.
Lisa Davies
December 18, 2025 AT 20:25This is so important!! 💪 Seriously, if you're on an SSRI and reach for Advil, pause. Just pause. Talk to your doc. Acetaminophen is your friend 🤝❤️
Benjamin Glover
December 19, 2025 AT 08:17A 75% increased risk? Pathetic. If you can't manage pain without toxic combinations, you're not managing your health-you're enabling it.
John Brown
December 20, 2025 AT 17:31I was on sertraline and took naproxen for my back for months. Never thought twice. Then I got black stools. ER. Two days in. PPI now. Never again. This post saved me from a worse outcome. Thanks for writing this.
Mike Nordby
December 22, 2025 AT 12:54The pharmacokinetic interaction between SSRIs and NSAIDs is well-characterized in the literature. Platelet serotonin reuptake inhibition combined with COX-1 suppression creates a synergistic impairment of hemostasis. The clinical implications are significant, particularly in elderly populations with polypharmacy. Prophylactic PPI use is supported by multiple randomized controlled trials.
Michelle M
December 22, 2025 AT 20:56It’s funny how we treat our bodies like machines you can just plug and play with pills. But we’re not circuits. We’re ecosystems. Serotonin doesn’t just live in your brain-it’s in your gut, your blood, your bones. When you mess with one part, the whole system feels it. This isn’t a drug interaction. It’s a wake-up call to see ourselves as whole.
Jake Sinatra
December 23, 2025 AT 15:23This is exactly why we need better patient education. I’ve seen too many cases where patients are discharged after GI bleeds without being told the cause. Doctors assume patients know. Patients assume doctors told them. Neither is true. This post should be required reading for anyone on antidepressants.