CYP450 Medication Interaction Checker
Check Your Medication Interactions
Enter medications you're taking to see if they interact through CYP450 enzymes. This tool is educational only and does not replace professional medical advice.
How This Works
CYP450 enzymes in your liver process 90% of medications. When two drugs compete for the same enzyme, one can be blocked or metabolized too quickly.
CYP450 Enzyme Chart
Results
Enter medications above to see interaction results.
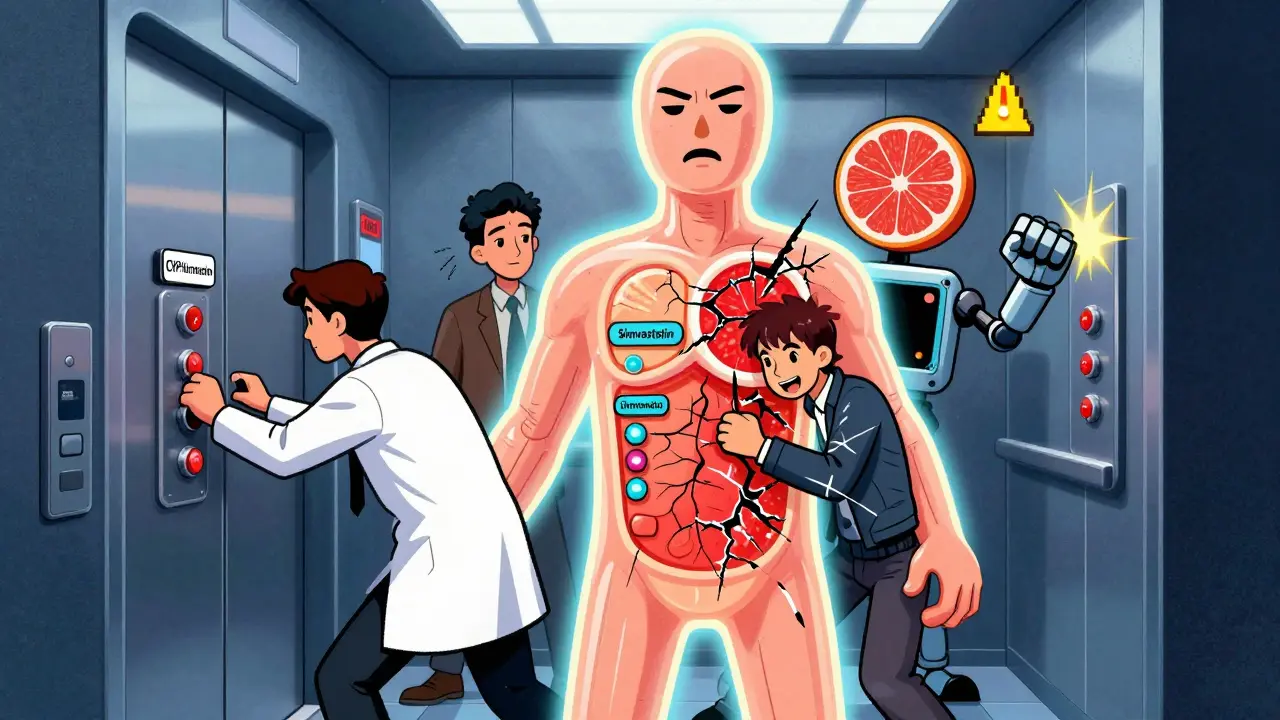
Why Your Medications Might Be Fighting Each Other
Your body doesn’t treat every drug the same way. Even if you’re taking two perfectly legal prescriptions, they could be competing for the same metabolic pathway-like two cars trying to use the same narrow tunnel at the same time. This isn’t just theoretical. It’s happening right now in millions of people, and it’s one of the most common reasons medications stop working-or cause serious side effects.
The main players in this hidden battle are the CYP450 enzymes. These proteins, mostly found in your liver and intestines, are responsible for breaking down about 90% of all prescription drugs. If you’re on statins, antidepressants, blood thinners, or even common painkillers, chances are your body is using one or more of these enzymes to process them. But here’s the catch: if two drugs need the same enzyme at the same time, one will win-and the other might not get processed at all.
Who’s Winning the Metabolic Race?
Not all CYP450 enzymes are created equal. Six of them handle the vast majority of drug metabolism. The biggest is CYP3A4, responsible for breaking down half of all medications-everything from cholesterol-lowering statins to heart medications and opioids. Next is CYP2D6, which handles a quarter of all drugs, including many antidepressants and beta-blockers. Then come CYP2C9, CYP2C19, CYP1A2, and CYP2E1, each managing smaller but still critical shares of the workload.
When two drugs target the same enzyme, the one with a stronger binding affinity takes priority. Think of it like a crowded elevator: the person who steps in first and holds the door open gets to stay. If you’re taking a drug that binds tightly to CYP3A4-like clarithromycin (an antibiotic)-it can block other drugs from getting processed. That’s why a 72-year-old woman on simvastatin ended up in the hospital with muscle breakdown after adding clarithromycin. Her simvastatin levels spiked tenfold because the enzyme couldn’t clear it anymore.
Two Ways Drugs Interfere: Inhibition and Induction
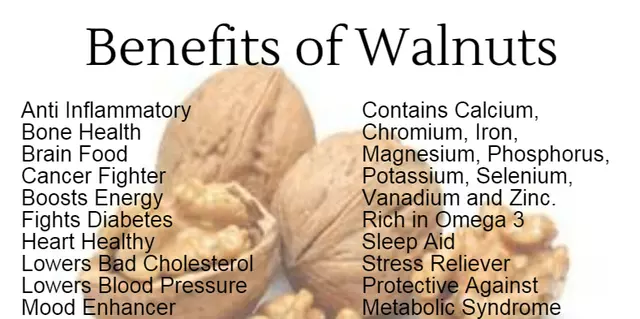
There are two main ways drugs disrupt CYP450 metabolism: inhibition and induction. Inhibition is like jamming the lock on the enzyme’s door. Some drugs, like grapefruit juice, can block CYP3A4 in your gut so effectively that drug absorption drops by up to 80%. This isn’t just a myth-it’s a documented risk with over 85 medications. Even a single glass of grapefruit juice can cause problems for days.
Other inhibitors, like fluvoxamine (an antidepressant), can shut down CYP1A2 so completely that theophylline (a lung medication) builds up to toxic levels. One patient’s theophylline levels jumped from 10 to 25 mcg/mL in under 48 hours-enough to trigger seizures.
Induction is the opposite. Some drugs, like rifampin (an antibiotic used for tuberculosis), don’t just block enzymes-they tell your body to make more of them. Within a week, CYP3A4 activity can increase by 400-600%. That means drugs metabolized by that enzyme get cleared too fast. Birth control pills, immunosuppressants, and even some pain meds become ineffective. A patient on cyclosporine after a kidney transplant could reject the organ if rifampin is added without adjusting the dose.
Genetics Play a Bigger Role Than You Think
Not everyone metabolizes drugs the same way. Your genes decide whether you’re a slow, normal, or super-fast metabolizer. For CYP2D6, about 5-10% of white people are poor metabolizers-they barely break down the drug at all. That means standard doses of antidepressants like amitriptyline can cause dangerous side effects. On the flip side, ultrarapid metabolizers (1-10% of people, depending on ancestry) process drugs so quickly they never reach therapeutic levels.
This isn’t just theory. A patient taking codeine for pain might feel nothing because their body converts it to morphine too fast-and then clears it just as fast. Meanwhile, another patient with the same prescription could overdose on morphine because they barely convert it at all. That’s why the FDA recommends genetic testing before prescribing clopidogrel, a blood thinner that needs CYP2C19 to activate. Thirty percent of Caucasians and 60% of Asians are slow metabolizers for this enzyme, making the drug useless for them.
Real-World Examples You Should Know
Here’s what this looks like in practice:
- SSRIs + beta-blockers: Fluoxetine and paroxetine inhibit CYP2D6. When combined with metoprolol, they can cause dangerously slow heart rates. Nurses report this interaction in 15-20% of patients.
- St. John’s wort + birth control: This herbal supplement induces CYP3A4. Women on birth control pills have reported unplanned pregnancies after starting it.
- Warfarin + antibiotics: CYP2C9 breaks down warfarin. Antibiotics like trimethoprim-sulfamethoxazole can inhibit it, causing bleeding. One study found 1 in 10 warfarin patients had a major bleed linked to a drug interaction.
- Opioids + antifungals: Ketoconazole blocks CYP3A4. When taken with fentanyl or oxycodone, it can cause respiratory depression-even at normal opioid doses.
These aren’t rare cases. They’re routine. And they’re preventable.
How Doctors and Pharmacists Are Fighting Back
Hospitals and pharmacies now use tools like Lexicomp and clinical decision support systems that flag dangerous combinations before a prescription is filled. These systems catch 95% of major interactions. Still, only 42% of pharmacists check for CYP450 interactions routinely-and only 28% of primary care doctors do.
Pharmacogenomic testing is becoming more common. Panels that check for CYP2D6, CYP2C9, CYP2C19, and other key enzymes now cost $250-$500 and take 3-7 days. Some academic medical centers have started offering these tests as standard before prescribing high-risk drugs. Insurance coverage is still spotty, but it’s improving.
Electronic health records are catching up too. Epic, Cerner, and Allscripts now send real-time alerts when a new prescription might clash with an existing one. One hospital system reported a 35% drop in CYP-related adverse events after implementing these alerts.

What You Can Do
You don’t need to be a scientist to protect yourself. Here’s what works:
- Keep a full list of everything you take-prescriptions, supplements, herbal products, even over-the-counter painkillers. Many people forget that ibuprofen can interfere with blood pressure meds.
- Ask your pharmacist every time you pick up a new prescription: “Could this interact with anything else I’m taking?” Pharmacists are trained for this. Use them.
- Know your grapefruit risk. If you’re on a statin, calcium channel blocker, or certain anti-anxiety drugs, avoid grapefruit entirely. It’s not worth the gamble.
- Watch for changes. If you start a new drug and suddenly feel dizzy, weak, nauseous, or unusually sleepy, call your doctor. It might not be the drug itself-it might be the interaction.
- Consider genetic testing if you’ve had bad reactions to medications before, or if you’re on multiple drugs for chronic conditions. It’s not expensive, and it can save your life.
The Bigger Picture
CYP450 interactions aren’t going away. In fact, they’re getting more common. The average Medicare patient takes 5.4 medications. That’s over 10 potential enzyme conflicts per person. And with more people living longer with multiple chronic conditions, the risk keeps rising.
Still, the future is brighter. AI tools like IBM Watson for Drug Interactions are getting better at predicting clashes before they happen. By 2025, the NIH plans to standardize how we name CYP450 gene variants-making it easier for doctors to interpret test results. And more drug labels now include clear warnings about CYP interactions.
The bottom line? Drug interactions aren’t a glitch. They’re a feature of modern medicine. But they’re not unavoidable. With awareness, simple checks, and smart communication with your care team, you can stay safe-even in a world where your medications are constantly fighting for space.
Can grapefruit juice really affect my medications?
Yes, and it’s one of the most dangerous food-drug interactions out there. Grapefruit juice blocks CYP3A4 in your intestines, which means drugs like simvastatin, atorvastatin, felodipine, and some anti-anxiety meds can build up to toxic levels. Even one glass can have an effect that lasts over 24 hours. If you’re on any medication, check if grapefruit is listed as a warning-then avoid it completely.
Are herbal supplements safe with my prescriptions?
Not necessarily. St. John’s wort induces CYP3A4 and can make birth control, antidepressants, and transplant drugs ineffective. Garlic, ginkgo, and goldenseal can also interfere with blood thinners and other medications. Just because something is "natural" doesn’t mean it’s safe with your prescriptions. Always tell your doctor or pharmacist what supplements you’re taking.
Why does my medication stop working after a few weeks?
It might not be your body getting used to it-it could be a new drug or supplement inducing CYP enzymes. Rifampin, certain antiseizure meds, and even smoking can speed up metabolism of drugs like oral contraceptives, antipsychotics, or blood thinners. If you notice your medication isn’t working like it used to, ask if anything new was added to your regimen.
Do I need genetic testing for CYP450 enzymes?
Not everyone does-but if you’ve had unexplained side effects, poor response to multiple drugs, or you’re on 3+ medications, it’s worth considering. Testing for CYP2D6, CYP2C9, and CYP2C19 can reveal if you’re a slow or fast metabolizer. This helps doctors choose the right drug and dose from the start. Costs are dropping, and more insurers are covering it for high-risk patients.
Can CYP450 interactions cause long-term damage?
Yes. Repeated exposure to drug interactions can lead to organ damage. For example, long-term statin buildup due to CYP3A4 inhibition can cause muscle breakdown (rhabdomyolysis), which can lead to kidney failure. Repeated low-level warfarin interactions can cause internal bleeding. These aren’t one-time accidents-they’re preventable patterns. The more drugs you take, the more important it is to monitor for these interactions.
Final Thought: Knowledge Is Your Shield
You don’t need to memorize every enzyme or drug interaction. But you do need to know that interactions happen-and that they’re not always obvious. The best defense? Stay informed, ask questions, and keep your care team updated. Your life might depend on it.





Justin Fauth
February 3, 2026 AT 14:52This is why America's healthcare is a dumpster fire. Doctors don't even check for this stuff. I had my dad on simvastatin and he took grapefruit juice like it was water. Ended up in the ER with rhabdo. Nobody warned him. Nobody. Just pure negligence.
Meenal Khurana
February 3, 2026 AT 15:14Grapefruit juice is dangerous with statins. Always check labels.
caroline hernandez
February 5, 2026 AT 13:26The CYP450 system is the unsung hero of pharmacokinetics. CYP3A4 alone handles over 50% of clinically relevant substrates, and its polymorphic nature-especially when combined with environmental inhibitors like furanocoumarins in grapefruit-creates a pharmacodynamic minefield. Patients on polypharmacy regimens are essentially walking biochemical experiments without informed consent. We need mandatory pharmacogenomic screening before initiating multi-drug protocols, especially in geriatric populations where polypharmacy prevalence exceeds 80%.
Joy Johnston
February 7, 2026 AT 02:03I work as a clinical pharmacist, and this is exactly why we mandate medication reconciliation at every visit. The CYP2D6 poor metabolizer phenotype is alarmingly common in Caucasian populations-up to 10%. When a patient presents with unexplained side effects from SSRIs or beta-blockers, we immediately consider pharmacogenetic factors. We’ve seen patients on paroxetine and metoprolol develop bradycardia so severe they required pacing. It’s preventable. Always ask your pharmacist. Always.
Shelby Price
February 7, 2026 AT 08:00so like... grapefruit = bad. got it. 🍊🚫💊
Jesse Naidoo
February 7, 2026 AT 10:05You know who’s really behind this? Big Pharma. They don’t want you to know how many drugs are designed to fail unless you’re on another drug they sell. That’s why they don’t test for interactions properly. They profit from side effects. I’ve seen it. They even hide genetic data from patients. Wake up.
Sherman Lee
February 8, 2026 AT 00:38LMAO at people who think this is "new info." 😂 I’ve been screaming about this since 2018. My cousin died from a CYP3A4 interaction with fentanyl + ketoconazole. The ER doctor said "it’s rare." RARE? It’s in the FDA’s black box warnings. But nooo, let’s just blame the patient for taking two meds. 🤡 #BigPharmaLies
Lorena Druetta
February 9, 2026 AT 12:28This is so important. If you’re taking more than three medications, please, please talk to your pharmacist. They are the quiet heroes of healthcare. You don’t need to be a scientist to save your life-just be brave enough to ask. Your life matters. 💛
Zachary French
February 11, 2026 AT 08:08Bro. I swear the FDA is just a glorified marketing dept for Big Pharma. They let this stuff slide because they want you to keep buying new drugs when the old ones "stop working." And don’t get me started on St. John’s Wort. It’s like nature’s version of a Trojan horse. 🤯 I took it with my Zoloft and felt like a zombie for a week. My doc said "it’s herbal, it’s fine." 😭
Daz Leonheart
February 11, 2026 AT 21:43This is gold. Seriously. I’ve been on 5 meds for years and never thought about how they might be fighting each other. I’m going to print this out and take it to my pharmacist tomorrow. Thank you for writing this. You just might have saved my life.
Kunal Kaushik
February 12, 2026 AT 02:35In India, we don’t even have access to pharmacogenetic testing. Most people just take what the doctor gives them. This post should be translated into Hindi and Tamil. So many people are at risk here. 🙏
Nathan King
February 12, 2026 AT 16:09The clinical implications of CYP450-mediated drug-drug interactions are not merely pharmacological but also ethical. The failure to integrate pharmacogenomic screening into standard-of-care protocols constitutes a systemic dereliction of duty, particularly in populations with high polypharmacy burdens. The current paradigm of reactive, symptom-based intervention is antiquated and perilous. Proactive, genotype-guided prescribing must be institutionalized.
Antwonette Robinson
February 13, 2026 AT 23:08Oh wow, so drugs can interact? Shocking. I bet next you’ll tell me water can drown people. 🙄
Ed Mackey
February 14, 2026 AT 00:49i just found out my blood pressure med and that ginkgo i took for "brain boost" were fighting. my head was spinning for weeks. i didnt even know to ask. thanks for the heads up. gonna start keeping a list now.