When you’ve been on a biologic drug like infliximab or adalimumab for years, your body knows the medicine. It works. You feel stable. Then your doctor says, "We’re switching you to a biosimilar." Suddenly, your mind races: What happens when you change from originator? Will your symptoms come back? Will you feel worse? Is this just a cost-cutting move disguised as medical advice?
What Exactly Is a Biosimilar?
A biosimilar isn’t a generic. That’s the first thing to understand. Generics are exact chemical copies of small-molecule drugs-like taking a different brand of ibuprofen. Biosimilars are copies of complex biologic drugs, which are made from living cells. Think of it like trying to recreate a handmade sweater. Even if you use the same yarn and pattern, the texture, drape, and feel might be slightly different. But if it keeps you warm just as well, does it matter? The U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) require biosimilars to show no clinically meaningful difference in safety, purity, or potency compared to the original. That means the same effectiveness, same side effect profile, same dosing. They’re not identical-no two batches of a biologic are-but they’re close enough that your body responds the same way. The first biosimilar approved in the U.S. was Zarxio (filgrastim-sndz) in 2015. Since then, 37 biosimilars have been approved, mostly targeting common conditions like rheumatoid arthritis, psoriasis, and inflammatory bowel disease. By 2023, about 70% of all biosimilar use in the U.S. was for tumor necrosis factor (TNF) inhibitors like infliximab and adalimumab.What Happens When You Switch?
Switching from an originator biologic to a biosimilar isn’t a leap into the unknown. It’s backed by data from over 80 clinical studies. The NOR-Switch trial, which followed 481 patients with inflammatory diseases for a year, found that switching from originator infliximab to its biosimilar CT-P13 resulted in similar disease control. Retention rates were 52.6% for the biosimilar group versus 60% for the originator group-but the difference wasn’t statistically significant. In other words, most people stayed on the treatment without problems. Real-world data from Denmark, Germany, and the U.S. consistently show that over 85% of patients remain on their biosimilar after 12 months. That’s the same retention rate as staying on the original drug. One key finding: switching doesn’t cause more side effects. In a 2022 study of 140 patients who switched multiple times-from originator to biosimilar to another biosimilar-immunogenicity (the body making antibodies against the drug) stayed low: only 3 cases per 100 patient-years. Trough levels (the amount of drug left in your blood between doses) didn’t change meaningfully. One patient’s infliximab level went from 4.3 μg/mL to 4.1 μg/mL after switching. That’s a drop of less than 5%. Not clinically relevant.Why Do Some People Stop Taking It?
Here’s the real issue: people stop not because the drug stops working, but because they think it will. A 2021 study in Frontiers in Psychology found that 32.7% of patients reported new or worsening symptoms after switching-even though lab tests and disease scores showed no change. This is called the nocebo effect: expecting something bad to happen makes you feel it. Reddit threads from patients with rheumatoid arthritis are full of posts like: “I switched to the biosimilar and suddenly I’m more tired. My joints ache again.” But when doctors checked their DAS28 scores (a standard measure of RA activity), everything was stable. Same with IBD patients who say, “My stools aren’t normal anymore.” Their fecal calprotectin levels? Still in remission range. Actual discontinuation due to real drug failure is rare. In studies, only 1.7% of patients stopped because of confirmed immunogenicity. Most stops-12% to 18%-are linked to perception, fear, or poor communication.
Who Shouldn’t Switch?
Switching works best for people with stable disease. If your RA is under control (DAS28 under 3.2), your IBD is in remission, and your psoriasis has cleared up-switching is safe and supported by guidelines from the FDA and EMA. But if you’re in the middle of a flare, or your disease is unpredictable, don’t switch. That’s not because biosimilars are riskier-it’s because changing anything during a flare makes it impossible to tell if the flare is from the disease or the switch. Also, avoid multiple switches. Switching once-from originator to biosimilar-is well-studied. Switching twice or three times? The data is thinner. One Spanish study found 15.3% of IBD patients stopped after switching from one biosimilar to another, compared to 8.7% in those who didn’t switch. Trough levels were fine, but something about the change triggered discontinuation. Maybe it’s the uncertainty. Maybe it’s the lack of trust.The Cost Difference Matters
Biosimilars cost 15% to 35% less than the original biologic. In 2023, when Humira biosimilars hit the U.S. market, they launched at a 35% discount. That’s billions saved for insurers and patients. In Europe, 67% of filgrastim use is biosimilar. In the U.S., it’s only 24% for infliximab. Why? Patent thickets, rebate deals, and pharmacy networks that favor originators. But health plans are catching on. By 2023, 85% of U.S. health plans had mandatory switch policies for certain biologics. That’s not just corporate cost-cutting. It’s about access. Many patients can’t afford the originator. A biosimilar makes treatment possible.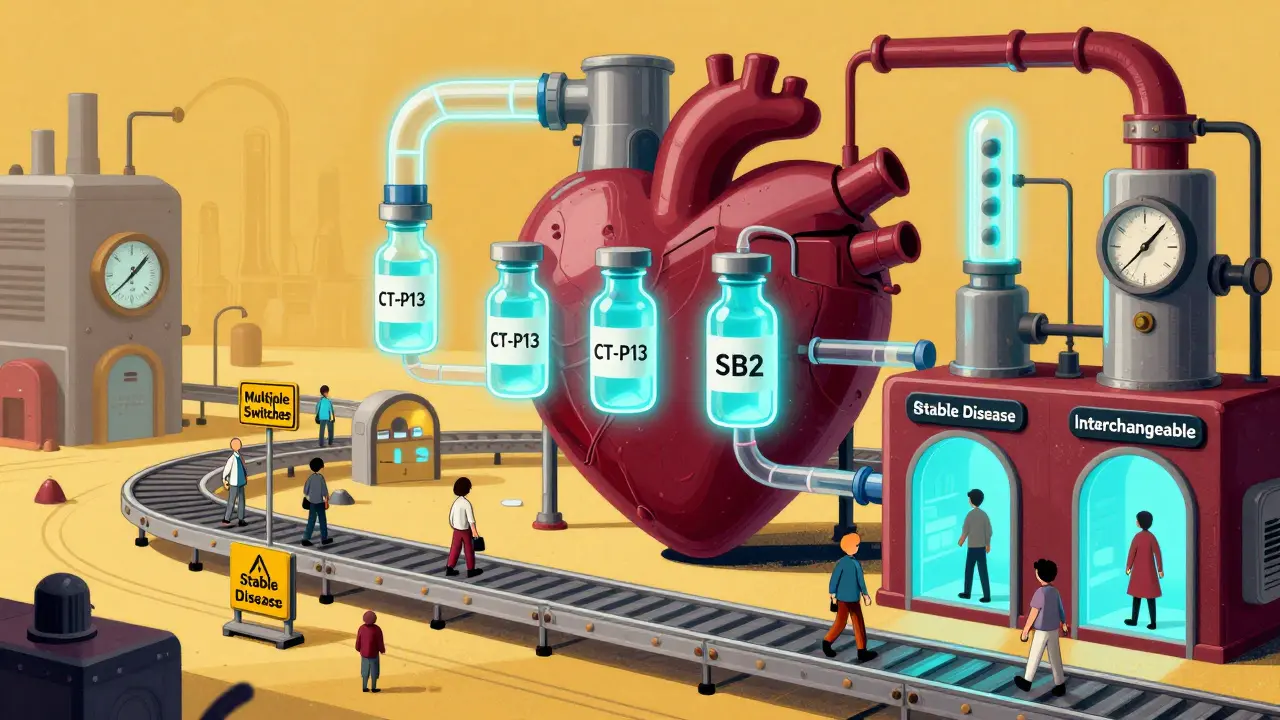
What Should You Do Before Switching?
Don’t just accept the switch. Ask for a conversation. A good provider will spend at least 20 minutes explaining:- Why you’re switching
- What the biosimilar is (and isn’t)
- What to expect-both good and bad
- How you’ll be monitored (DAS28, PASI, trough levels, etc.)
- When to call if you feel off
Interchangeability: The Next Step
In 2024, the FDA approved the first interchangeable adalimumab biosimilar: Cyltezo. That means pharmacists can swap it for the originator without asking your doctor. It’s like switching from brand-name Advil to generic ibuprofen-but for a complex biologic. This is huge. It means easier access, less paperwork, lower cost. But it also means less control. Some patients worry about being switched without their knowledge. That’s why clear communication before the switch matters more than ever.Bottom Line
Switching from an originator biologic to a biosimilar is safe for most people with stable chronic disease. The science says so. The real-world data says so. The regulatory agencies say so. The biggest risk isn’t the drug. It’s fear. Misinformation. Poor communication. If you’re being asked to switch, don’t panic. Ask questions. Get data. Know what’s normal. Track how you feel. And remember: you’re not being replaced. You’re being given the same effective treatment at a lower cost. The goal isn’t to switch everyone. It’s to make life-changing treatments available to everyone. And that’s worth getting right.Is switching from an originator biologic to a biosimilar safe?
Yes, for most patients with stable disease. Data from over 80 clinical studies, including the NOR-Switch trial and multiple real-world cohorts, show no clinically meaningful difference in safety, efficacy, or immunogenicity when switching from originator biologics like infliximab or adalimumab to their biosimilars. Retention rates remain above 85% at 12 months, and serious adverse events are no more common than with the original drug.
Why do some patients feel worse after switching?
Most patients who feel worse after switching are experiencing the nocebo effect-where expectations of negative outcomes lead to real symptoms, even when the drug is working. Studies show up to 33% of patients report new symptoms after a switch, but lab tests and disease activity scores often show no change. Psychological support and clear communication before the switch can reduce this by more than half.
Can you switch between different biosimilars?
Yes, but with more caution. Switching once-from originator to biosimilar-is well-supported by evidence. Switching between biosimilars (e.g., from CT-P13 to SB2) has less data, though studies like Lauret et al. (2022) show immunogenicity remains low and drug levels stay stable. Some real-world studies report slightly higher discontinuation rates after multiple switches, likely due to patient anxiety rather than drug failure.
Are biosimilars cheaper than the original drugs?
Yes. Biosimilars are typically priced 15% to 35% lower than their originator counterparts. For example, Humira biosimilars launched in the U.S. at a 35% discount in 2023. These savings help reduce costs for insurers, pharmacies, and patients, and increase access to treatment for people who couldn’t afford the original biologic.
Who should avoid switching to a biosimilar?
Patients with active disease flares, unstable conditions, or recent treatment changes should avoid switching until their disease is stable. Also, patients who have had multiple prior switches or who are highly anxious about the change may benefit from staying on their current drug. Always discuss your individual situation with your doctor before switching.
What’s the difference between a biosimilar and a generic?
Generics are exact chemical copies of small-molecule drugs, like aspirin or metformin. Biosimilars are highly similar-but not identical-to complex biologic drugs made from living cells, like infliximab or adalimumab. Because biologics are made in living systems, they can’t be copied exactly. Biosimilars must prove they work the same way through extensive testing, but minor differences in inactive ingredients are allowed.
Can a pharmacist switch my medication without telling me?
Only if your biosimilar is designated as "interchangeable" by the FDA-like Cyltezo for adalimumab. In those cases, pharmacists can substitute it without asking your doctor. But many states require pharmacies to notify patients or providers when a substitution occurs. Always check your state’s rules and ask your pharmacist if you’re unsure.
How long should I wait to see if the biosimilar is working?
Give it at least 3 months. Biologics take time to reach steady state in your body. Your doctor should check your disease activity score (like DAS28 for arthritis or PASI for psoriasis) and possibly your drug trough level around the 12-week mark. If you’re feeling worse before then, report it-but don’t assume it’s the drug. Stress, infections, or other factors can cause temporary flares.





Ellie Norris
February 3, 2026 AT 03:59Okay but like… I switched from Humira to a biosimilar last year and honestly? My joints didn’t care. I was scared too, but my DAS28 stayed the same and my insurance saved like $800/month. My rheumatologist said if it ain’t broke, don’t fix it-but mine was kinda broke before, so this was a win. Also, no more ‘biologic’ label on my prescription, which is weirdly satisfying. 😅
Marc Durocher
February 4, 2026 AT 15:57Bro. I switched three times. Originator → biosimilar A → biosimilar B. My trough levels? Same. My symptoms? Same. My anxiety? Skyrocketed. I swear my body knows when the pill bottle looks different. Not because the drug changed-but because my brain screamed ‘SCAM’. The science says it’s fine. My nerves say ‘prove it’. 🤷♂️
larry keenan
February 5, 2026 AT 15:09The clinical data supporting biosimilar switching is robust, particularly with regard to pharmacokinetic equivalence and immunogenicity profiles. The NOR-Switch trial demonstrated non-inferiority in disease control metrics, and real-world retention rates exceeding 85% suggest clinical utility. However, the nocebo effect remains a significant confounder in patient-reported outcomes, necessitating structured patient education protocols prior to transition.
Nick Flake
February 5, 2026 AT 22:13Imagine your body is a garden. The originator? The exact soil, the exact sun, the exact rain. The biosimilar? Same plants. Same nutrients. But the gardener’s hands are different. You don’t know if it’s the hands-or if you just *think* they’re different. That’s the nocebo. That’s the fear. That’s the silent war inside us. 🌱💔 We’re not afraid of the drug. We’re afraid of losing control. And that? That’s the real illness.
Akhona Myeki
February 7, 2026 AT 06:26Let me be clear: in South Africa, we do not have access to these expensive biologics at all. You people complain about switching to a biosimilar? We are grateful for any treatment that doesn’t cost a kidney. Your privilege is showing. This isn’t about preference-it’s about survival. Stop whining and be grateful your system even allows this.
Chinmoy Kumar
February 8, 2026 AT 19:42hey i switched last year and i was super nervous but now i feel better than before? idk maybe it was the extra sleep or my dog stopped barking at night but my psoriasis cleared up even more. maybe the biosimilar is just… better? or maybe i just stopped stressing about it. sometimes the mind is the real medicine. 🙏
Brett MacDonald
February 9, 2026 AT 06:46so like… if the drug is 99.9% the same, why does it feel different? is it the fillers? the packaging? the fact that the bottle has a different color? or is it just… our brains are wired to panic when things change? i think we’re scared of being lab rats. and honestly? fair.
Sandeep Kumar
February 9, 2026 AT 20:33Biosimilars are just generics with a fancy name. Big Pharma wants you to pay less so they can charge more elsewhere. Trust the system? Nah. Trust your body. Stay on the original. They’ll never admit it but they’re just trying to cut corners.