It’s easy to assume that if you’re taking medications as prescribed, you’re safe. But what if your blood pressure pill starts acting like a stimulant? Or your antidepressant makes you feel like you’re burning up from the inside? These aren’t just bad days - they could be signs of a drug interaction.
Drug interactions happen when one medication changes how another works in your body. It could be two prescription drugs, a prescription and an over-the-counter pill, or even your daily vitamin with your heart medication. The result? A drug might become too strong, too weak, or trigger side effects you’ve never seen before. The U.S. Food and Drug Administration says these interactions can make your medicine less effective, cause unexpected reactions, or even turn a mild drug into a dangerous one.
Every year in the U.S., over 1.3 million people end up in the emergency room because of adverse drug reactions. About 350,000 of those cases require hospitalization. And here’s the scary part: nearly 40% of these reactions are preventable. That means if you know what to look for, you might avoid a trip to the hospital entirely.
Symptoms That Require Immediate Emergency Care
Some drug interactions don’t wait. They strike fast and can kill you within minutes. If you experience any of these, call emergency services right away - don’t wait, don’t text your doctor, don’t Google it.
- Difficulty breathing or oxygen levels below 90% (measured by a pulse oximeter). This is common in severe allergic reactions and can mean your airway is closing.
- Swelling of the face, lips, tongue, or throat. This is called angioedema. It can block your airway completely in under 20 minutes.
- Heart racing over 120 beats per minute while your blood pressure drops below 90. This combination signals anaphylactic shock - your body is shutting down.
- Seizures lasting longer than 2 minutes or sudden loss of consciousness. This can happen with overdose of certain painkillers, antibiotics, or even some herbal supplements.
- Body temperature above 41°C (106°F), rigid muscles, and extreme agitation. This is serotonin syndrome - often triggered by mixing antidepressants with pain meds like tramadol or fentanyl.
These aren’t "maybe" symptoms. They’re red flags. A 2022 study from Emergency Medicine Cases found that 1-2% of people taking multiple serotonergic drugs develop serotonin syndrome. That might sound rare, but when it hits, 40% of those patients end up in the ICU. Don’t gamble with it.
Symptoms That Need Medical Attention Within 24 Hours
Not every interaction screams for an ambulance. But if you ignore these signs for too long, they can turn into something serious - or even permanent.
- A widespread rash covering more than 30% of your skin, especially if it’s red, blistering, or peeling. This could be DRESS syndrome - a delayed reaction that attacks your liver, kidneys, and blood cells.
- Unexplained fever over 38.5°C (101.3°F) lasting more than 48 hours. This is common with antibiotics like sulfonamides or anticonvulsants like carbamazepine. It’s not a cold - it’s your immune system going haywire.
- Unusual bruising or bleeding. If your platelet count drops below 100,000/μL, even a minor bump can cause internal bleeding. This happens with some antibiotics, diuretics, and even herbal products like ginkgo biloba.
- Yellow eyes or skin, dark urine, or belly pain. These are signs your liver is damaged. ALT levels over 120 U/L mean your liver is under stress. Drug-induced liver injury is rare - only 1 in 10,000 to 100,000 cases - but it’s the leading cause of sudden liver failure in the U.S.
- Little or no urine output for 6+ hours, especially if your creatinine level has jumped. This could mean your kidneys are failing from a drug reaction. About 1 in 5 cases of acute kidney injury in hospitals are caused by medications.
One patient on Reddit shared how he took a common antibiotic for a sinus infection and developed a rash and fever. He waited three days, thinking it was "just a virus." By the time he went to the ER, his liver enzymes were 15 times higher than normal. He spent two weeks in the hospital.
What Makes Some Interactions More Dangerous Than Others?
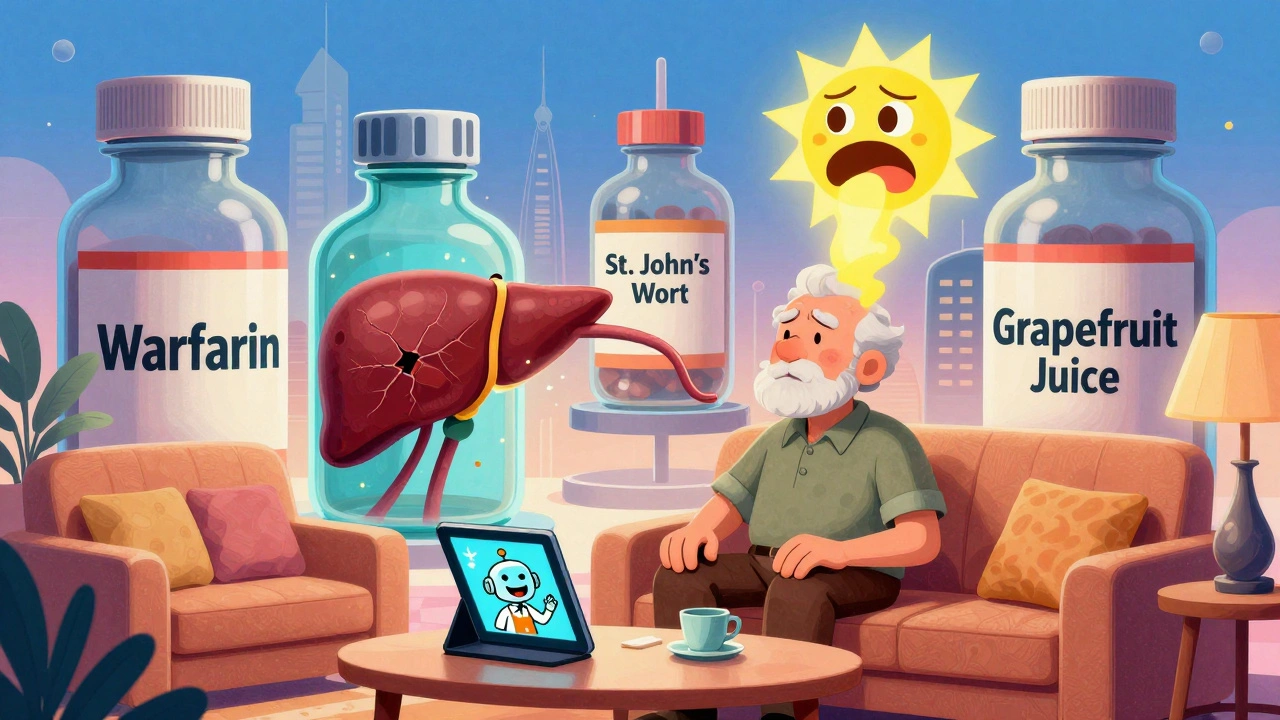
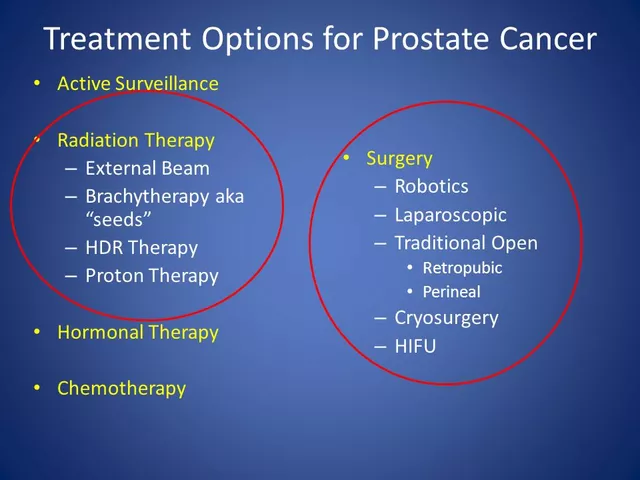
Not all drugs are created equal. Some have a "narrow therapeutic index" - meaning the difference between a safe dose and a toxic one is tiny. Even a small change in how your body processes the drug can be deadly.
Drugs like warfarin (a blood thinner), digoxin (for heart failure), and phenytoin (for seizures) fall into this category. A 20% change in blood levels can mean the difference between preventing a clot and causing a stroke - or between controlling seizures and triggering toxicity.
These drugs are especially risky when mixed with:
- Antibiotics like clarithromycin or fluconazole
- Herbal supplements like St. John’s wort
- Foods like grapefruit juice
Studies show that 78% of primary care doctors use digital interaction checkers like Lexicomp or Micromedex. But here’s the problem: 47% of them say they ignore warnings because they get too many false alerts. That’s called "alert fatigue." You can’t rely on your doctor to catch everything. You need to know the signs yourself.
Why Most People Wait Too Long to Get Help
A 2022 survey of 1,200 patients found that 58% waited more than 12 hours before calling their doctor after noticing symptoms like dizziness, nausea, or unusual fatigue. Why? Because they thought it was "just a side effect," "stress," or "getting older."
Another study from JAMA Internal Medicine found that 68% of patients couldn’t recognize serious interaction symptoms from the medication leaflets they were given. Those papers are written for pharmacists, not patients. They use terms like "hepatotoxicity" and "QT prolongation." You’re not supposed to understand them.
But you don’t need to. You just need to know your body. If something feels wrong - not just uncomfortable, but off - trust it. That gut feeling? It’s your body’s early warning system.
What to Do If You Suspect a Drug Interaction
Don’t panic. Don’t stop your meds cold unless you’re having a life-threatening reaction. Do this instead:
- Stop taking the new medication or supplement you started recently - but only if it’s safe to do so. Never stop blood thinners, seizure meds, or heart meds without medical advice.
- Telephone your doctor or pharmacist. Call poison control if you’re unsure. In the U.S., it’s 1-800-222-1222. In New Zealand, call Healthline at 0800 611 116. They’re trained to handle these calls.
- Observe your symptoms. Write them down: when they started, what you took, how bad they are, and if anything made them better or worse.
- Present all your medications - including vitamins, herbal teas, CBD oil, and over-the-counter painkillers - to your doctor. People forget about the "little" stuff, but 18% of serious interactions involve supplements.
There’s a tool called the "STOP" protocol used by Kaiser Permanente. It’s simple, effective, and designed for people who aren’t medical experts. Use it.

How to Prevent Drug Interactions Before They Happen
Prevention is always better than emergency care. Here’s how to stay safe:
- Keep a full list of everything you take - prescription, OTC, supplements, and even herbal remedies. Update it every time you start or stop something.
- Use one pharmacy for all your prescriptions. They can flag interactions across all your meds. If you use multiple pharmacies, they won’t see the full picture.
- Ask your doctor or pharmacist: "Could this interact with anything else I’m taking?" Don’t assume they know your full list. Say it out loud.
- Check for grapefruit. It interferes with more than 85 medications - including statins, blood pressure drugs, and some anxiety meds. If your pill bottle doesn’t warn you about it, ask.
- Use a reliable interaction checker. Drugs.com and the Liverpool Drug Interaction Group are free, updated daily, and include supplements. Don’t trust random apps.
People on five or more medications have a 57% chance of a major interaction. If you’re over 65, that number goes even higher. That’s not aging - that’s a system failure. You have to be your own advocate.
What Happens After You Seek Help?
If you go to the ER with suspected drug interaction, they’ll likely:
- Check your vital signs: heart rate, blood pressure, oxygen, temperature
- Run blood tests: liver enzymes, kidney function, electrolytes, drug levels
- Ask for a full medication list - bring the bottles
- Stop the suspected drug(s) and monitor you
- Give supportive care: IV fluids, oxygen, or antidotes if available
The Council of International Organizations of Medical Sciences (CIOMS) scale helps doctors confirm if a reaction is truly drug-related. They look for three things: Did symptoms start after taking the drug? Did they get better when you stopped it? And if you took it again, did they come back? If yes to all three - it’s a confirmed interaction.
And here’s the good news: If you catch it early, you often don’t need hospitalization. The American Association of Poison Control Centers reports that 65% of interaction cases are managed successfully over the phone. You don’t always need an ER visit - just a quick call.
Final Thought: Your Body Knows Before You Do
Medications save lives. But they also carry risk. And that risk goes up the more you take. The average person over 65 is on seven medications. That’s seven chances for something to go wrong.
Don’t wait until you’re gasping for air or your skin is peeling off. If something feels off - if you feel different, weaker, hotter, or just plain wrong - act. Call your doctor. Call poison control. Don’t wait for someone else to tell you it’s serious.
Your health isn’t a guessing game. It’s your life. And you’re the only one who knows your body well enough to spot when something’s not right.
What are the most common drugs that cause dangerous interactions?
The most dangerous interactions involve drugs with a narrow therapeutic index - meaning small changes in blood levels can be life-threatening. These include warfarin (blood thinner), digoxin (heart medication), phenytoin (seizure control), and lithium (mood stabilizer). They’re often affected by antibiotics, antifungals, grapefruit juice, and herbal supplements like St. John’s wort. Even common OTC painkillers like ibuprofen can increase bleeding risk when taken with warfarin.
Can herbal supplements cause drug interactions?
Yes, and they’re often overlooked. St. John’s wort can reduce the effectiveness of birth control pills, antidepressants, and HIV medications. Ginkgo biloba and garlic supplements can increase bleeding risk when taken with blood thinners like warfarin. Even turmeric and ginger can interfere with blood sugar control in people taking diabetes medications. About 18% of serious drug interactions involve herbal products, according to the National Institutes of Health.
Is it safe to take two OTC painkillers together?
Not always. Many OTC painkillers contain the same active ingredient. For example, taking Tylenol (acetaminophen) with a cold medicine that also has acetaminophen can lead to accidental overdose - the leading cause of acute liver failure in the U.S. Always check the "Active Ingredients" section on the label. Never combine pain relievers unless your doctor says it’s safe.
What should I do if I miss a dose and then take two pills by accident?
Don’t panic, but don’t ignore it either. Call your pharmacist or poison control immediately. For most medications, taking one extra pill won’t cause harm. But for drugs like insulin, blood thinners, or seizure meds, even one extra dose can be dangerous. Keep your medication list handy when you call - they’ll need to know exactly what you took and how much.
Can drug interactions happen with foods or drinks?
Absolutely. Grapefruit juice is the most well-known - it can make statins, blood pressure meds, and some anxiety drugs too strong, leading to dangerous side effects. Alcohol can worsen drowsiness from sedatives or antidepressants. High-sodium foods can reduce the effect of blood pressure medications. Even leafy greens high in vitamin K can interfere with warfarin, making it less effective at preventing clots.
How do I know if my symptoms are from a drug interaction or just a virus?
Ask yourself: Did these symptoms start within hours or days of taking a new medication or changing a dose? If yes, it’s likely related. Viruses usually cause fever, cough, sore throat - not sudden confusion, chest pain, or skin peeling. If you’re on multiple medications and feel unwell, assume it’s the meds until proven otherwise. Better to get checked than to wait.
Are drug interactions more common in older adults?
Yes. People over 65 are more likely to take five or more medications, and their bodies process drugs differently - slower liver and kidney function means drugs stay in the system longer. Studies show 45% of adults over 65 take five or more drugs, and they have a 57% risk of a major interaction. Age isn’t the problem - polypharmacy is. That’s why regular medication reviews with your doctor are critical.





Ibrahim Yakubu
December 6, 2025 AT 12:53Bro, I took gabapentin with tramadol last year and woke up screaming in a hotel room thinking my skin was melting. No joke. ER said serotonin syndrome. They gave me benzodiazepines and I cried for 3 hours. You think your doctor knows? Nah. They just write scripts. You gotta be your own damn watchdog.
Gwyneth Agnes
December 8, 2025 AT 02:22Stop taking everything.
olive ashley
December 9, 2025 AT 12:21Oh great, another fearmongering post from someone who thinks every pill is a landmine. I’ve been on 8 meds since I was 22 and I’ve never had an interaction. You know why? Because I don’t take random supplements from Amazon. St. John’s wort? That’s not medicine, that’s a cult. And grapefruit juice? If you’re on statins, you’re already dumb enough to need this post. Congrats, you’ve scared people who don’t even know what a CYP3A4 enzyme is.
Also, ‘body temp above 41°C’? That’s a medical emergency regardless of meds. You don’t need a 2000-word essay to tell people to call 911 if they’re burning up. This is just fear porn wrapped in stats.
Priya Ranjan
December 11, 2025 AT 02:49It’s not fear porn-it’s survival. You think your body is invincible because you’re young? I’ve seen people die from mixing ibuprofen with warfarin because they thought ‘it’s just painkillers.’ Your arrogance is what kills people. You don’t get to be the exception. Not when the data says 40% of these are preventable.
And yes, St. John’s wort is dangerous. It’s not a ‘cult.’ It’s a CYP450 inhibitor. If you don’t know what that means, maybe you shouldn’t be mixing supplements with prescriptions. But hey, keep living dangerously.
Mansi Bansal
December 12, 2025 AT 20:12One must contemplate, with grave seriousness, the epistemological vacuum that permits laypersons to self-administer polypharmaceutical regimens without adequate pharmacovigilance. The modern pharmacopeia is a labyrinth of biochemical interdependencies, and the casual consumer, armed with nothing but a Google search and a Walmart loyalty card, is akin to a child wielding a chainsaw.
St. John’s wort, a botanical agent of profound serotonergic modulation, is routinely conflated with ‘natural wellness’-a dangerously fallacious construct. Its interaction with SSRIs is not anecdotal; it is codified in the British National Formulary, the Lexicomp database, and the FDA’s Adverse Event Reporting System.
Furthermore, the normalization of ‘just taking an extra Tylenol’ is a public health catastrophe. Acetaminophen hepatotoxicity is silent, insidious, and irreversible. The liver does not scream before it fails.
It is not fearmongering to insist upon diligence. It is the bare minimum of human responsibility.
Nigel ntini
December 12, 2025 AT 22:45I get why this post exists. And I’m glad it does. But let’s not turn every side effect into a horror movie. I’ve been on blood pressure meds for 15 years, add in a daily fish oil, a magnesium, and melatonin-and I’ve never had an issue. Why? Because I use one pharmacy, I keep a list, and I ask my pharmacist every time something changes.
That’s the real takeaway here: it’s not about being paranoid. It’s about being organized. The system isn’t broken-you’re just not using the tools that are already there.
And yes, grapefruit juice ruins statins. But if your doctor doesn’t tell you that, find a new one. Not all of us need to live in fear. Just in awareness.
Brooke Evers
December 13, 2025 AT 15:58I just want to say thank you for writing this. I’m a nurse, and I’ve seen too many people come in with liver failure because they took ‘just one’ extra pill of Tylenol with their cold medicine. Or they started turmeric because their friend said it ‘cleanses the body’-and then their blood thinners stopped working. No one told them.
It’s not about scaring you. It’s about giving you the power to speak up. If you feel off, it’s not ‘just stress.’ It’s your body screaming. And if your doctor brushes you off? Go to another one. Or call poison control. They’re free, they’re trained, and they won’t make you feel dumb.
I’ve had patients cry because they waited too long. Please don’t be one of them. You’re not overreacting. You’re being smart.
And if you’re on five or more meds? Write them all down. Keep the bottles. Take them to every appointment. Even the gummy vitamins. Even the ‘natural’ sleep aids. They’re not harmless. They’re chemicals. And your body remembers every one.
You’re not alone. We’re here. We see you. And we want you to be okay.
Kumar Shubhranshu
December 15, 2025 AT 15:18My uncle died from DRESS syndrome after taking sulfamethoxazole. He didn’t know. His doctor didn’t know. The hospital didn’t know. He was 52. Just a rash. Just a fever. Just a bad cold. Now he’s gone. Don’t wait. Call now.
Max Manoles
December 15, 2025 AT 18:33One thing no one talks about: the pharmacy techs. They see everything. They see the 87-year-old woman who’s on 14 meds and the 22-year-old who’s stacking OTC sleep aids with antidepressants. They’re the ones who flag the interactions your doctor misses.
So next time you’re picking up a script, ask them: ‘Hey, does this mess with anything else I take?’ They’re not just bagging your pills-they’re saving your life. And they’re paid minimum wage to do it.
Don’t be too proud to ask. They’ve seen worse.
Andrew Frazier
December 16, 2025 AT 16:04Y’all act like Americans are dumb for taking meds. Meanwhile in India, people take 7 pills at once with chai and call it ‘Ayurveda.’ No one’s writing posts about that. Why? Because you’re scared of the truth. This post is just woke medicine for people who think ‘natural’ means safe. Wake up.
Ashish Vazirani
December 16, 2025 AT 17:09AMERICA! You think you're safe because you have a doctor? HA! In India, we have 12 medicines in one tablet-no labels, no warnings, just ‘take one after dinner.’ And we live longer! You think grapefruit juice is dangerous? We drink it with blood pressure pills and it makes us strong! Your system is broken because you’re weak! You need to stop being so scared of your own bodies! We don’t have time for your ‘alert fatigue’! We have to survive!
My cousin took 10 paracetamol with whiskey and danced for 3 days. He’s fine. You think you’re special? You’re just soft.
Karen Mitchell
December 18, 2025 AT 09:04This is a classic example of medical overreach. If you're taking seven medications, the problem isn't the interaction-it's the prescribing. Why are you on so many drugs in the first place? The real issue is pharmaceutical capitalism. You're being monetized, not healed.
Stop blaming the patient. Start blaming the industry.
Rashmi Gupta
December 19, 2025 AT 18:32Actually, the most dangerous interaction is trusting this post. Real doctors don’t scare people with 41°C temperatures-they assess context. You’re not a lab report. You’re a person. And if you’re panicking over every new symptom, you’re the problem, not the pills.