Digital Therapy Overview
When working with digital therapy, a clinically supported software‑based treatment that delivers therapeutic interventions through digital devices. Also known as digital therapeutics, it blends technology with health care. Another key player is telemedicine, remote clinical services via video or chat. Mobile health apps such as mHealth apps, applications on smartphones that track health data and guide behavior power many programs. Virtual CBT, a form of online cognitive behavioral therapy, delivers structured therapy sessions through the web, rounds out the ecosystem.
Digital therapy digital therapy encompasses virtual CBT, remote monitoring, and games designed to improve cognition. It requires reliable internet, user‑friendly interfaces, and evidence‑based content. Regulatory bodies influence the field; for example, the FDA’s digital health program reviews safety and efficacy data before a product can claim therapeutic benefit. This creates a trust loop: clinicians rely on approved tools, patients gain confidence, and insurers consider coverage. The result is a growing catalog of prescription‑grade apps that can be prescribed alongside traditional medication.
Evidence shows that patients using digital therapy achieve comparable outcomes to face‑to‑face treatment for anxiety, depression, and chronic disease management. Clinical trials often report reduced symptom scores within weeks, and meta‑analyses highlight cost savings of up to 30 % compared with standard care. These findings attract healthcare providers who seek scalable solutions for high‑volume conditions. Moreover, real‑world data from mHealth platforms feed back into research, sharpening algorithms and personalizing interventions.
Data security is another pillar. Because digital therapy collects sensitive health information, platforms must comply with HIPAA, GDPR, or local privacy laws. Encryption, secure authentication, and transparent consent processes protect users and reduce legal risk. When patients see that their data are safe, adherence improves, and the therapeutic loop strengthens.
Patient adherence often hinges on engagement features. Gamified progress tracking, push notifications, and peer support communities boost daily usage. Studies link higher engagement to better clinical results, reinforcing the need for well‑designed user experiences. Developers therefore collaborate with psychologists, designers, and engineers to craft interventions that feel like everyday apps rather than medical chores.
Healthcare providers benefit from integrated dashboards that summarize patient progress, flag non‑adherence, and suggest next steps. This data‑driven approach lets clinicians intervene early, adjust treatment plans, and document outcomes for insurance claims. The synergy between digital therapy and traditional visits creates a hybrid model where technology augments, rather than replaces, professional judgment.
Why Digital Therapy Matters
In summary, digital therapy brings together telemedicine, mobile health apps, and virtual CBT into a cohesive ecosystem that expands access, lowers costs, and maintains clinical quality. Whether you’re a patient looking for a convenient way to manage symptoms, a clinician exploring prescription‑grade apps, or a stakeholder interested in the regulatory landscape, the collection below offers detailed comparisons, safety tips, and purchasing guides for a wide range of digital health products. Dive into the articles to see how each solution fits into the broader picture of modern, technology‑enabled care.
 24 September 2025
24 September 2025
Schizophrenia and Tech: Top Apps & Online Resources That Help
Explore how smartphones, wearables, and web platforms empower people with schizophrenia to track symptoms, stay connected, and access evidence‑based care.
Latest Posts
-

Anticoagulants for Seniors: When Stroke Prevention Outweighs Fall Risk
-

How to Use Label Information to Set Accurate Medication Reminders
-
When to Seek Medical Help for a Suspected Drug Interaction
-
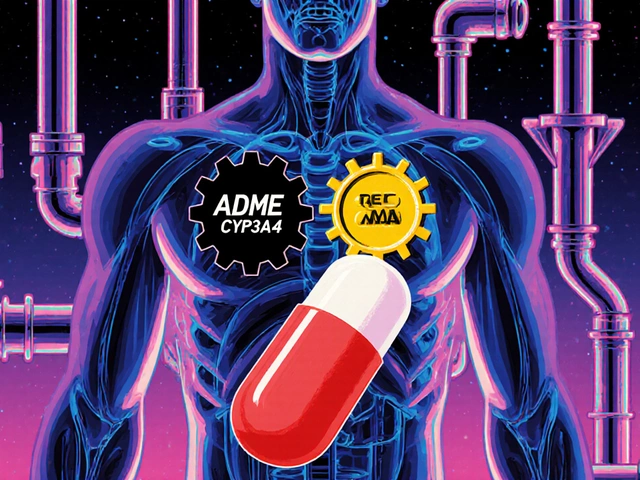
Pharmacokinetic vs Pharmacodynamic Drug Interactions: What You Need to Know
-
The Role of Hiccups in Detoxification and Cleansing

20