Cross-Reactivity: What It Is and How It Affects Medications and Allergies
When your body mistakes one thing for another—like confusing a drug for a food protein—that’s cross-reactivity, a biological response where the immune system reacts to similar structures across different substances. Also known as cross-allergy, it’s why someone allergic to peanuts might react to lupin, or why a penicillin allergy could make you sensitive to certain cephalosporins. This isn’t just about food or drugs—it’s about molecular similarities that trick your immune system into thinking something harmless is dangerous.
It shows up in unexpected places. For example, if you’re allergic to shellfish, you might react to iodine-based contrast dyes—not because iodine causes allergies, but because proteins in shellfish look enough like molecules in the dye to trigger a response. The same thing happens with biosimilars, medications designed to mimic biologic drugs. Even though they’re highly similar, tiny structural differences can cause immune systems to react differently, especially if you’ve had prior exposure to the original drug. Then there’s drug allergy, an immune-mediated reaction to a medication. Cross-reactivity here explains why some people can’t take certain antibiotics, painkillers, or blood pressure meds after reacting to one drug in the same class. It’s not just about the drug itself—it’s about the shape of its molecules and how your body remembers them.
It’s not always obvious. A person might think they’re allergic to aspirin, but the real issue is cross-reactivity with other NSAIDs like ibuprofen. Or someone with a latex allergy might react to bananas, avocados, or kiwis because those foods share similar proteins. Even food allergy, an immune response triggered by specific proteins in food can cross over into medication reactions—like when a soy allergy affects how your body handles certain injectables or fillers in pills. This is why doctors ask about every allergy, even ones that seem unrelated.
Understanding cross-reactivity helps you avoid unnecessary reactions, unnecessary drugs, and unnecessary fear. It’s why some people get rashes after switching from brand-name drugs to generics—not because the generic is bad, but because of subtle differences in inactive ingredients or manufacturing that trigger a cross-reaction. It’s also why desensitization therapy works for some with sound sensitivity or immune overreactions: your brain and immune system can be retrained to stop seeing harmless things as threats.
What you’ll find in the posts below are real cases where cross-reactivity changes treatment outcomes—whether it’s a patient reacting to azilsartan because of a prior ACE inhibitor reaction, someone with MS having a pseudorelapse after eating shellfish, or a person with hyperacusis whose brain misfires because of past noise trauma. These aren’t random stories. They’re clues to how your body connects the dots between things that seem unrelated—and how to break those connections before they hurt you.
 3 February 2026
3 February 2026
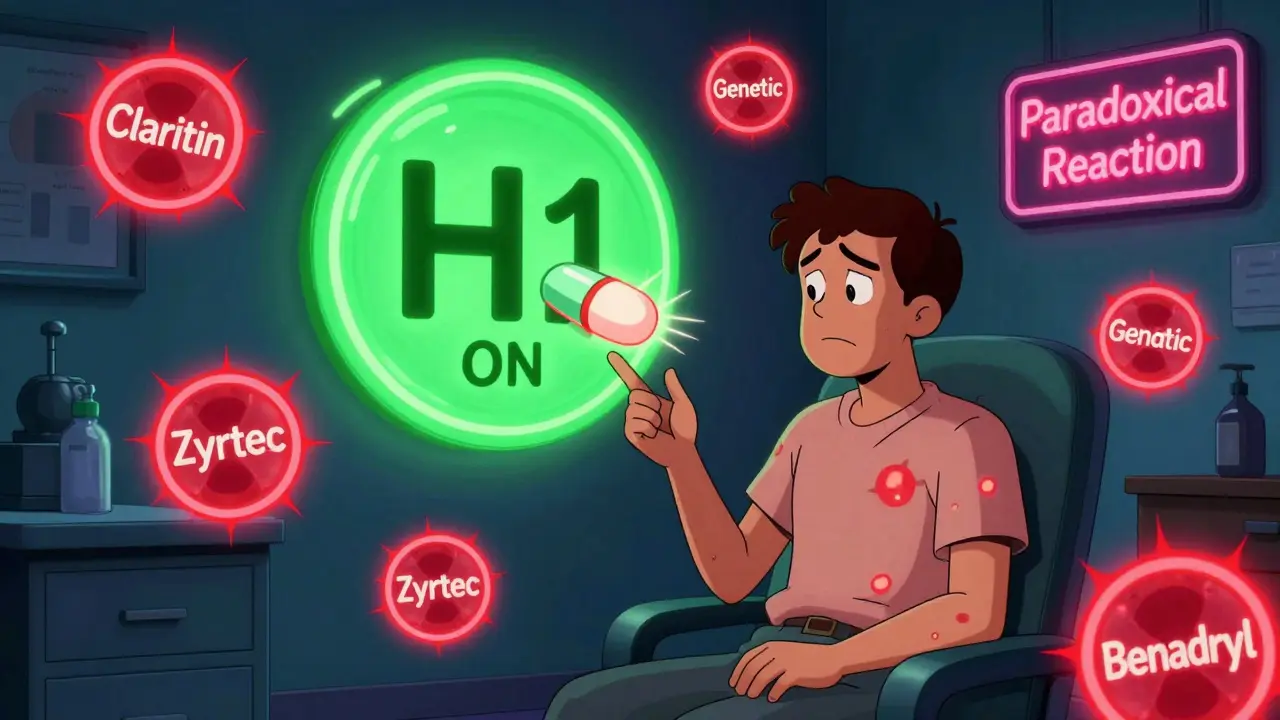
Antihistamine Allergies and Cross-Reactivity: What to Watch For
Some people develop allergic reactions to antihistamines themselves, making their symptoms worse instead of better. This rare condition, called antihistamine hypersensitivity, can occur with any common drug like Zyrtec or Benadryl. Learn what causes it, how to recognize it, and what to do next.
 23 November 2025
23 November 2025
Latex Allergy: Cross-Reactivity and Workplace Management
Latex allergy affects 1-2% of the population and up to 12% of healthcare workers. Learn about cross-reactive foods, how powdered gloves spread allergens, and how workplaces can create safe environments with non-latex alternatives.
Latest Posts
-

Top Alternatives to Northwest Pharmacy: Finding the Best Online Pharmacies in 2024
-

Extra Super Avana (Dapoxetine & Avanafil) vs. Other ED & Premature Ejaculation Options
-

PCSK9 Inhibitors vs Statins: Side Effects and Outcomes
-

Long-Acting Injectables: Why Extended Side Effect Monitoring Can’t Be Ignored
-

Import Inspections: How the FDA Monitors Drugs Entering the US

12