Brand Name Drugs: What They Are, Why They Cost More, and When Generics Work Just as Well
When you hear brand name drugs, the original versions of medications developed and marketed by pharmaceutical companies under a patent-protected name. Also known as originator drugs, they’re the first to hit the market after years of research and testing. These are the pills you see advertised on TV—Lipitor, Nexium, Cialis Super Active. They’re not magic. They’re just the first version of a drug that proved safe and effective in clinical trials. But here’s the catch: once the patent runs out, anyone can make the same thing. That’s where generic drugs, chemically identical versions of brand name drugs sold at lower prices after patent expiration come in.
So why do brand name drugs cost so much more? It’s not because they work better. It’s because the company that made them spent millions on research, clinical trials, and marketing. They need to recoup that money before competitors can copy the formula. But once generics enter the market, prices drop—often by 80% or more. That’s why switching from brand name to generic can save you hundreds or even thousands a year, especially for chronic conditions like high blood pressure, depression, or diabetes. And studies, including those from the FDA and independent medical journals, show generics work just as well. The active ingredient is the same. The body absorbs it the same way. The only differences are in the fillers, color, or shape—things that don’t affect how the drug works.
But it’s not always that simple. Some people notice changes when switching, especially with thyroid meds, drugs like levothyroxine where tiny differences in absorption can impact hormone levels, or blood thinners, like warfarin or DOACs, where even small variations in how the drug is absorbed can affect clotting risk. That’s why keeping a medication journal, a simple log tracking how you feel after switching to a new generic version matters. It’s not paranoia—it’s smart self-advocacy. If you feel off after a switch, write it down. Talk to your doctor. Your report could help uncover a real, if rare, issue with a specific manufacturer’s version.
Big pharma doesn’t always make it easy. Some companies use legal tricks—like pulling the original brand off the market or changing the pill just enough to reset the patent clock—to delay generics. This is called product hopping, a strategy where drugmakers slightly alter a medication to avoid generic competition. It’s not illegal, but it’s controversial. That’s why the FTC and consumer groups are pushing back. Meanwhile, you’re stuck paying more than you should. The good news? You have power. You can ask for generics. You can appeal insurance denials. You can report side effects to the FDA’s MedWatch system. Your voice helps keep the system honest.
Brand name drugs aren’t bad. They saved lives and set the standard. But they’re not always the best choice for your budget or your body. The real question isn’t whether generics work—it’s whether you’re getting the best value for your health. Below, you’ll find real stories and data from people who’ve switched, struggled, or fought for the right drug. Whether you’re dealing with high prices, weird side effects, or confusing insurance rules, there’s something here that speaks to your situation. No fluff. Just what you need to know to make smarter choices.
 6 December 2025
6 December 2025
Authorized Generic Pricing: Why They Cost Less Than Brand Name Drugs
Authorized generics are identical to brand-name drugs but cost significantly less because they skip marketing and branding expenses. Learn how they work, why they're cheaper, and how to get them.
Latest Posts
-

Top Alternatives to Northwest Pharmacy: Finding the Best Online Pharmacies in 2024
-

Color Blindness: Understanding Red-Green Defects and How They're Inherited
-

Questions to Ask Your Doctor Before Starting a New Medication
-

Authorized Generic Pricing: Why They Cost Less Than Brand Name Drugs
-
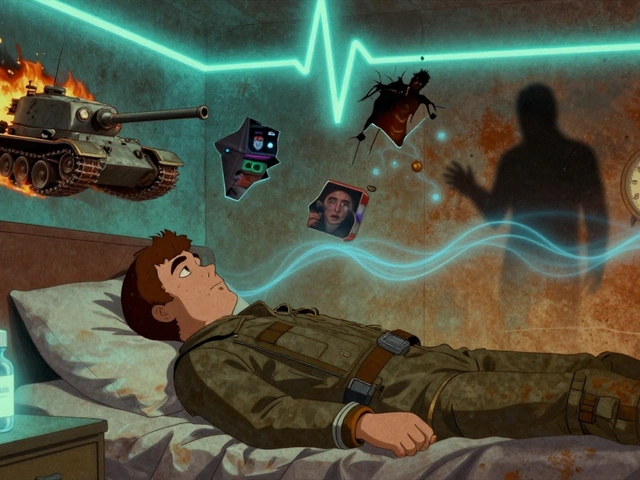
PTSD Nightmares: How Prazosin and Sleep Therapies Really Work

13