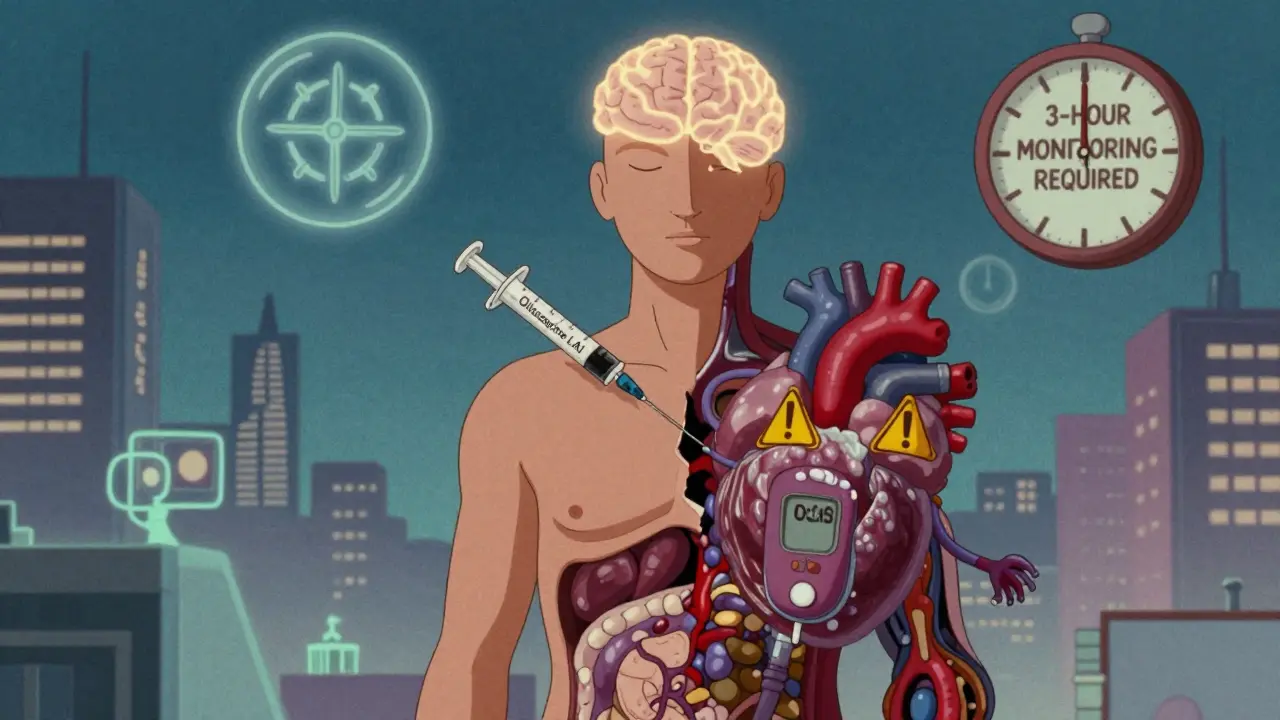
LAIs Side Effect Monitoring Guide
Why Monitoring Matters
Long-acting injectables (LAIs) are a lifeline for many with serious mental health conditions, but they carry significant side effects that can become serious if not monitored. 55% of patients on LAIs receive no documented side effect checks. This tool helps you track potential side effects and stay informed about essential monitoring requirements.
Common Side Effects
Essential Monitoring Guidelines
Before every injection: Blood pressure, heart rate, temperature
At every visit: Weight, waist circumference
Every 6 months: Fasting glucose, lipid panel, prolactin levels
Every 3 months: AIMS test (for involuntary movements)
Olanzapine-specific: 3-hour post-injection observation
Personal Monitoring Log
Track your own metrics between appointments to help your provider catch issues early
When you’re managing schizophrenia or another serious mental health condition, taking a pill every day can be hard. For many, long-acting injectables (LAIs) are a lifeline. These shots-given every few weeks or even months-keep medication levels steady, cut relapse rates by up to half, and mean fewer daily reminders of illness. But here’s the problem no one talks about enough: long-acting injectables come with serious, slow-burning side effects that can wreck your physical health if no one’s watching closely.
What LAIs Actually Do-and What They Hide
Long-acting injectables aren’t magic. They’re designed to release antipsychotic drugs slowly into your bloodstream, so you don’t have to remember daily pills. Common ones include paliperidone (Invega Sustenna), aripiprazole (Abilify Maintena), olanzapine (Zyprexa Relprevv), and haloperidol. They work. Studies show people on LAIs are 30-50% less likely to end up back in the hospital than those on oral meds. But every injection brings hidden risks. Some side effects show up fast-dizziness, drowsiness, high fever. Others creep in over months: weight gain, high blood sugar, high cholesterol, irregular heartbeat, even uncontrolled body movements you can’t stop. These aren’t rare. In fact, they’re common enough that the FDA requires specific monitoring for each drug. Take olanzapine LAI. It’s one of the most effective, but it carries a black box warning-the strongest possible-from the FDA. After every shot, you must be monitored for three full hours. Why? Because some people develop sudden, dangerous sedation or confusion. There have been deaths linked to this. And yet, in many clinics, that three-hour window is skipped because staff are short on time or training.The Monitoring Gap: 55% of Patients Are Left in the Dark
A 2021 audit of 5,169 patients on LAIs across 62 UK mental health services found something shocking: only 45% had any documented side effect check in the past year. That means more than half of people on these long-term shots were never checked for weight gain, blood pressure, blood sugar, or movement disorders. Let that sink in. You get a shot every six weeks. You see your doctor regularly. But no one asks if your pants are tighter. No one checks your cholesterol. No one uses the Abnormal Involuntary Movement Scale (AIMS) to see if you’re developing tardive dyskinesia-a condition where your face, tongue, or limbs move uncontrollably. And once it starts, it might never go away. Why does this happen? Two big reasons. First, time. Most appointments are 15 minutes. Clinicians are pressured to focus on mood, hallucinations, or aggression-the “mental” symptoms. Physical side effects? They’re an afterthought. One community psychiatrist on Reddit said it plainly: “I have 15 LAI patients. Only 15 minutes per appointment. I prioritize symptoms because that’s what gets reimbursed.” Second, training. A 2023 survey of 200 mental health nurses found that 62% felt unprepared to monitor LAI side effects. Most only checked for immediate injection pain or swelling. Few knew how to interpret prolactin levels, spot early signs of metabolic syndrome, or recognize neuroleptic malignant syndrome-a rare but deadly reaction that can kill within hours if untreated.Not All LAIs Are the Same-Here’s What You Need to Watch For
Each LAI has its own risk profile. You can’t treat them the same way.- Paliperidone (Invega Sustenna): Causes weight gain in most patients-average 4.2 kg in six months. Up to 70% develop high prolactin levels, leading to sexual dysfunction, missed periods, or breast growth. Requires blood tests every 6 months for glucose, lipids, and prolactin.
- Aripiprazole (Abilify Maintena): Better for weight and metabolism, but 20-25% get akathisia-restlessness so severe it feels like you can’t sit still. Often mistaken for worsening psychosis.
- Haloperidol (Haldol Decanoate): Older, cheaper, but causes movement problems in 30-50% of users. Tremors, stiffness, shuffling walk. Needs AIMS checks every month, not quarterly.
- Olanzapine (Zyprexa Relprevv): Highest risk for metabolic issues-diabetes, obesity, heart disease. Requires mandatory 3-hour post-injection monitoring. Also the most likely to cause sedation.
- Vital signs checked before every injection (temperature, heart rate, blood pressure)
- Weight and waist measurement at every visit
- Fast glucose and lipid panel every 6 months
- AIMS test every 3 months (monthly if high risk)
- Questions about sexual function, mood changes, and movement issues
What Works: The Clinics That Are Doing It Right
It’s not impossible. Some places have fixed this. The National Council’s LAMs program tracked 15 community centers that implemented structured LAI monitoring. They added 15-20 minutes to each appointment. Nurses were trained to use AIMS. Doctors had checklists. Patients got reminders to track their own symptoms between visits. Result? Hospitalizations dropped by 40%. Patients stayed on their meds longer. Side effects were caught early. One woman who gained 30 pounds on Invega Sustenna said, “No one asked about my weight until they started the new program. By then, my blood sugar was sky-high. If they’d checked earlier, I could’ve changed my diet. I wouldn’t have needed insulin.” These clinics didn’t need new drugs. They didn’t need more money. They just needed to stop assuming side effects would fix themselves.What’s Changing in 2025-2026
Change is coming-but slowly. The FDA is considering expanding its REMS (Risk Evaluation and Mitigation Strategy) program to include more LAIs beyond olanzapine. Medicare Advantage plans now tie reimbursement to LAI monitoring metrics. If you don’t document weight, blood pressure, and glucose, you don’t get paid. Digital tools are helping. Apps that send patients daily prompts to log fatigue, hunger, or twitching are being tested. Early results show a 30% increase in side effect reporting. Telehealth check-ins between injections are now recommended by the American Psychiatric Association. And there’s hope on the horizon: a blood test in phase 2 trials (NCT05214587) could predict who’s likely to gain weight on LAIs before they even start. That means doctors could pick a different drug upfront-instead of waiting for the scale to climb.
What You Can Do Now
If you or someone you care about is on a long-acting injectable, here’s what to demand:- Ask for a written monitoring plan. It should list what tests are done, how often, and who’s responsible.
- Keep your own log: weight, waist size, mood, sleep, movement issues. Bring it to every appointment.
- Ask: “Have you checked my blood sugar or cholesterol this year?” If they say no, push back.
- Request the AIMS test. It’s simple: the clinician watches your hands, tongue, and shoulders for involuntary movements. Takes two minutes.
- If you’re on olanzapine LAI, insist on the full 3-hour observation after injection. Don’t let them rush you out.
Why This Matters Beyond the Clinic
This isn’t just about individual patients. It’s about the system. LAIs are growing fast. The global market hit $5.8 billion in 2023 and is expected to hit $8 billion by 2030. More people will be on them. More people will develop diabetes, heart disease, or irreversible movement disorders. If we don’t fix monitoring now, we’re not just failing patients-we’re creating a future where psychiatric care is linked to chronic physical illness. And that’s a cost no health system can afford.What’s Next
The International Consortium on Schizophrenia Outcomes just released a 2024 global standard for LAI monitoring. It’s due to roll out in 2026. Until then, don’t wait for the system to catch up. Be the one who asks the hard questions. Be the one who writes down the numbers. Be the one who refuses to let a shot be the only thing that matters.Do long-acting injectables cause weight gain?
Yes, some do-especially olanzapine and paliperidone. On average, patients gain 4-8 kg (9-18 lbs) in the first 6 months. Aripiprazole has the least weight gain risk. Regular weight checks every visit and metabolic blood tests every 6 months are critical to catch this early.
How often should I get my blood tested on an LAI?
You should get fasting blood glucose and lipid panels every 6 months. If you’re on a high-risk LAI like olanzapine or paliperidone, or if you already have diabetes or high cholesterol, your doctor should test every 3 months. Prolactin levels should be checked at least once a year, especially if you’re experiencing sexual side effects or missed periods.
What is the AIMS test, and why is it important?
The Abnormal Involuntary Movement Scale (AIMS) is a 12-item clinical tool that checks for tardive dyskinesia-uncontrollable movements of the face, tongue, arms, or legs. It’s quick, takes less than 5 minutes, and should be done every 3 months. If caught early, stopping or switching the medication can prevent permanent damage. Many clinics skip it because it’s not billed separately, but it’s essential.
Can I refuse the 3-hour monitoring after an olanzapine injection?
No, you cannot legally refuse it if you’re receiving Zyprexa Relprevv. The FDA requires it because of documented cases of sudden, life-threatening sedation or confusion after injection. Even if you feel fine, you must stay under observation for 3 hours. This is not optional-it’s a safety rule backed by deaths.
Why don’t doctors check for side effects more often?
Most appointments are too short-often 15 minutes or less. Clinicians are pressured to focus on psychiatric symptoms because those are what get reimbursed by insurance. Physical side effects like weight gain or high blood sugar aren’t tracked in billing codes, so they’re deprioritized. Lack of staff training and poor documentation systems make it worse. But this is changing as value-based care models tie payments to monitoring quality.
Are there alternatives if I can’t tolerate LAI side effects?
Yes. If you’re having severe side effects, talk to your doctor about switching to a different LAI. Aripiprazole has fewer metabolic risks. Risperidone LAI may be better if movement issues are a problem. Some patients return to oral medications with adherence support like pill organizers or smartphone reminders. Others use long-acting oral formulations, which are being developed. Never stop or switch without medical guidance.




Angela Fisher
January 4, 2026 AT 00:54They're hiding the truth again. LAIs are just the start. They're testing mind control drugs on us under the guise of 'treatment'. The FDA? A puppet. The 3-hour monitoring? A cover so they can watch your vitals and feed data to Big Pharma. I've seen it. People disappear after their third shot. They don't die from illness. They die because their blood sugar drops too low... and no one writes it down. #MindControl #BigPharmaLies
Neela Sharma
January 5, 2026 AT 05:38This is the silence that kills We treat the mind like a broken vase But forget the body is the vase's clay A shot every six weeks But no one asks if you can breathe If your legs still remember how to walk If your heart still beats without fear We call it care But it's just convenience dressed in white coats You deserve more than a shot You deserve to be seen Not just monitored But held
Sarah Little
January 7, 2026 AT 02:04The clinical data is unequivocal: metabolic syndrome incidence in LAI cohorts exceeds 62% within 12 months, particularly with olanzapine and paliperidone formulations. Current monitoring protocols are non-compliant with ACC/AHA guidelines for metabolic risk stratification. Lack of standardized AIMS administration and inconsistent lipid panel timing represents a systemic failure in risk mitigation infrastructure. Without mandatory EHR-integrated alerts and reimbursement alignment, this remains a preventable iatrogenic epidemic.
JUNE OHM
January 7, 2026 AT 14:15America is being poisoned by these shots 🤢💉 They don't care about you. They care about profit. Olanzapine? Made in China. FDA? Bought and paid for. They let you get fat, diabetic, and twitching-then bill you for insulin and therapy. This is why I won't let my kid near a psychiatrist. They're not healers. They're chemists with licenses. We need a revolution. Not more meds. More truth. 🇺🇸🔥
Philip Leth
January 8, 2026 AT 15:28I'm from Nigeria, and here we don't even have LAIs. But I've seen family members on oral meds struggle daily. Your post hit me hard. In the U.S., you have access to all this tech and science, yet you're still falling through the cracks. It's not just about medicine-it's about dignity. If you're getting a shot every six weeks, you deserve more than a rushed check-in. You deserve someone who remembers your name, your weight, your fear. This isn't just healthcare. It's humanity.
Angela Goree
January 10, 2026 AT 03:16I've been on Invega for 3 years. They weighed me once. Said I 'looked fine.' My waist went from 32 to 40 inches. My A1C hit 7.8. No one asked. No one cared. I brought my log. They said, 'We'll add it to your file.' They never did. Now I'm on insulin. And guess what? They still don't check my AIMS. I'm not 'non-compliant.' I'm ignored. This system is broken. And I'm not the only one.
Shanahan Crowell
January 11, 2026 AT 13:25I used to think LAIs were just a tool. Now I see them as a mirror. They show us how little we value the whole person. We fix the mind, but let the body rot. But change is possible. I work in a clinic that started doing weekly weight checks, monthly AIMS, and patient-led symptom logs. We didn't get extra funding. We just started caring more. And guess what? People stayed. They trusted us. It's not about money. It's about showing up. Fully.
Kerry Howarth
January 11, 2026 AT 21:32Every LAI patient should receive a written monitoring plan signed by their provider. Weight, blood pressure, glucose, lipids, prolactin, and AIMS are non-negotiable. Documentation must be in the EHR with timestamps. If your clinic doesn't do this, ask for a referral. Your life depends on it.
Tiffany Channell
January 13, 2026 AT 18:35Of course they're skipping monitoring. It's cheaper. People who take LAIs are already seen as 'difficult' or 'non-compliant.' Why waste time on lab work when you can just up the dose? The real issue isn't the drugs-it's the patients who dare to live. They want you quiet, compliant, and chemically sedated-not healthy. You think this is about care? It's about control.