Stent Thrombosis Risk Calculator
This tool calculates your relative risk of stent thrombosis based on blood pressure levels. According to clinical studies, uncontrolled hypertension increases thrombosis risk by 1.5-2x compared to normal blood pressure.
How we calculate risk: Your risk is based on clinical studies showing that uncontrolled hypertension (≥130/80 mmHg) increases stent thrombosis risk by 1.5-2x compared to normal blood pressure.
For example: If your risk is 1.8x, this means you have an 80% higher chance of developing stent thrombosis compared to someone with normal blood pressure.
When a coronary stent is placed, the goal is to keep the artery open for the rest of a patient’s life. Yet a hidden danger can loom: a clot forming inside that tiny metal mesh. Stent thrombosis is the acute formation of a blood clot within a previously implanted coronary stent, often leading to heart attack or sudden cardiac death. While many factors play a role, one that’s frequently overlooked is high blood pressure. Understanding why hypertension fuels clot risk can help doctors and patients take smarter steps.
What is Stent Thrombosis?
Stent thrombosis typically occurs within the first month after a Percutaneous coronary intervention (PCI), but late events can happen years later. The clot, composed of activated platelets and fibrin, blocks the artery at the exact spot where the stent resides. There are three clinical categories:
- Acute (< 24 hours)
- Sub‑acute (24 hours‑30 days)
- Late/very late (> 30 days)
Each timeline reflects slightly different underlying mechanisms, yet the common denominator is an environment that encourages platelet adhesion.
Hypertension: The Silent Vessel Stressor
Hypertension is a sustained elevation of arterial blood pressure, typically defined as systolic ≥ 130 mmHg or diastolic ≥ 80 mmHg. It’s not just a number on a cuff; it reshapes the arterial wall, disrupts endothelial function, and creates turbulent flow-conditions ripe for clot formation.
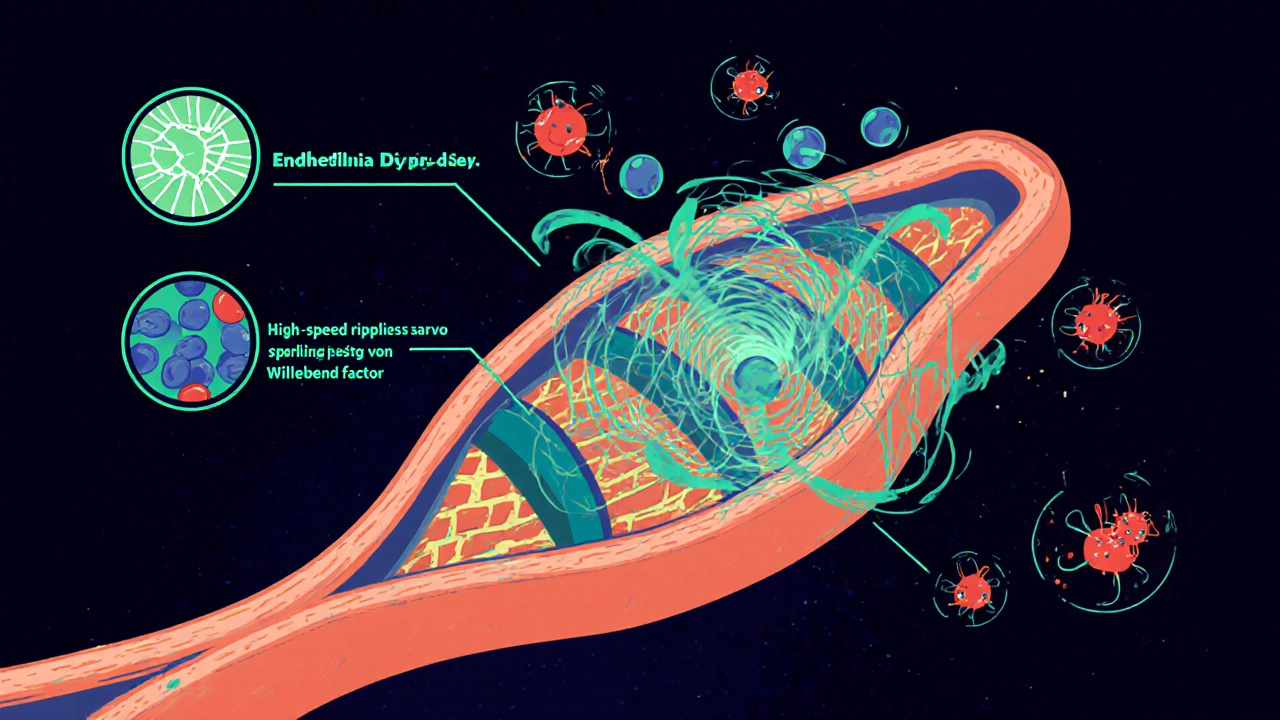
How High Blood Pressure Fuels Clot Formation in Stents
Three intertwined pathways explain the link:
- Endothelial dysfunction: High pressure damages the thin inner lining of the artery, reducing nitric oxide production. Without nitric oxide, platelets become more “sticky.”
- Increased shear stress: Elevated pressure raises the speed of blood passing through a narrowed segment. Shear stress activates von Willebrand factor, which captures circulating platelets on the stent struts.
- Inflammatory cascade: Hypertension triggers chronic low‑grade inflammation, raising levels of C‑reactive protein and fibrinogen-both prime ingredients for a clot.
When a stent is introduced, the metal surface itself can act as a scaffold for these activated platelets. If the surrounding artery is already compromised by hypertension, the clot‑forming process accelerates.
Clinical Evidence: Numbers That Matter
Large registry data from the United States and Europe consistently show a 1.5‑ to 2‑fold increase in stent thrombosis among patients with uncontrolled hypertension. A 2023 meta‑analysis of 12 studies (over 45 000 PCI patients) reported:
- Annual stent thrombosis rate: 0.4 % in normotensive vs. 0.8 % in hypertensive groups.
- Mortality after thrombotic events: 22 % vs. 12 % (hypertensive vs. normotensive).
These figures underscore that blood pressure control is not a side note-it’s a core part of stent longevity.
Key Risk Factors for Stent Thrombosis
| Risk Factor | Mechanism | Relative Impact* |
|---|---|---|
| Hypertension | Endothelial injury, shear stress, inflammation | 1.8× |
| Diabetes mellitus | Hyperglycemia‑induced platelet hyper‑reactivity | 1.5× |
| Incomplete dual antiplatelet therapy | Reduced inhibition of platelet aggregation | 2.2× |
| Complex lesion morphology | Irregular flow, larger metal surface area | 1.7× |
| Smoking | Oxidative stress, increased fibrinogen | 1.4× |
*Relative impact is expressed as odds ratio compared with a baseline patient without the risk factor.
Managing the Hypertension‑Stent Link
Effective risk reduction hinges on three pillars: medication, lifestyle, and vigilant monitoring.
1. Optimized Antihypertensive Regimen
Guidelines now recommend first‑line agents that also improve endothelial health, such as ACE inhibitors or ARBs. Adding a calcium‑channel blocker can further blunt shear‑stress spikes during physical activity.
2. Dual Antiplatelet Therapy (DAPT)
Standard DAPT-aspirin plus a P2Y12 inhibitor (e.g., clopidogrel, prasugrel, or ticagrelor)-should be maintained for at least 6-12 months after drug‑eluting stent placement. In hypertensive patients, extending DAPT to 12 months has shown a modest but statistically significant reduction in late thrombosis.
3. Lifestyle Adjustments
- Salt reduction: Cut daily sodium to < 2 g.
- Weight control: Aim for a BMI < 25 kg/m².
- Regular aerobic exercise: 150 minutes/week of moderate activity improves vascular compliance.
- Smoking cessation: Eliminates an independent pro‑thrombotic trigger.
4. Imaging Follow‑up
In selected high‑risk patients, intravascular ultrasound (IVUS) or optical coherence tomography (OCT) can detect early neointimal hyperplasia or uncovered stent struts, prompting earlier intervention.
Practical Checklist for Patients with Stents and High Blood Pressure
- Measure blood pressure at home twice daily; keep the average below 130/80 mmHg.
- Never skip an aspirin dose; set daily reminders.
- Take your P2Y12 inhibitor exactly as prescribed; discuss any side‑effects with your cardiologist.
- Schedule a follow‑up visit at 1 month, 3 months, and then annually to review BP and platelet therapy.
- Report any new chest discomfort, sudden shortness of breath, or palpitations immediately.

When Things Go Wrong: Recognizing Early Signs of Stent Thrombosis
Sudden, crushing chest pain radiating to the left arm or jaw, especially within the first month after PCI, should trigger an emergency call. Even in the “late” phase, atypical symptoms-such as unexplained fatigue or mild dyspnea-may hint at a partial blockage. Prompt angiography can save the heart and the patient.
Future Directions
Researchers are testing bio‑resorbable stents that dissolve after the artery heals, potentially reducing the long‑term clot risk. Meanwhile, novel antithrombotic agents that target specific pathways activated by high shear stress are in phase III trials. Until those become mainstream, strict blood pressure control remains the most practical weapon.
Frequently Asked Questions
Can normal‑range blood pressure still cause stent clots?
Even a mildly elevated systolic pressure (130‑139 mmHg) increases shear stress enough to promote platelet activation on stent struts. Keeping pressure consistently below 130/80 mmHg is associated with the lowest thrombosis rates.
Do ACE inhibitors reduce stent clot risk?
Yes. ACE inhibitors improve endothelial function and lower arterial pressure, both of which blunt the mechanisms that lead to clot formation. Studies show a 12‑% relative risk reduction in stent thrombosis when patients are on an ACE inhibitor versus no renin‑angiotensin blockade.
How long should I stay on dual antiplatelet therapy if I have hypertension?
Guidelines recommend at least 12 months for drug‑eluting stents in hypertensive patients, especially if other risk factors (diabetes, smoking) are present. Your cardiologist may tailor the duration based on bleeding risk.
Is there a test to see if my stent is at risk of clotting?
Advanced imaging like IVUS or OCT can visualize uncovered struts or thin‑cap fibroatheroma around the stent, which are early warning signs. Routine blood tests for platelet reactivity are also available but not yet standard practice.
Should I avoid intense exercise after getting a stent?
Mild to moderate aerobic activity is encouraged because it improves vascular health. However, very high‑intensity bursts can spike blood pressure sharply; discuss a safe exercise plan with your cardiologist.
In short, high blood pressure isn’t just a number on a chart-it directly reshapes the environment inside a coronary stent, making clots more likely. By pairing aggressive blood pressure control with optimal antiplatelet therapy and lifestyle tweaks, patients can dramatically lower the odds of a life‑threatening event.






Brandy Eichberger
October 21, 2025 AT 13:10Reading through the recent synthesis on hypertension and stent thrombosis feels like perusing a finely crafted symphony of pathophysiology.
The author deftly navigates endothelial dysfunction, shear stress, and inflammation with a clarity that would make any cardiologist swoon.
One cannot help but appreciate the meticulous citation of the 2023 meta‑analysis, which anchors the narrative in robust data.
While many laypeople might skimp on the nuance of nitric oxide deficiency, the piece foregrounds its centrality with commendable precision.
Moreover, the delineation of risk stratification-acute, sub‑acute, late-offers a pedagogical scaffold for both trainees and seasoned interventionalists.
The practical checklist, replete with home‑monitoring protocols, transcends mere academic discourse and ventures into actionable guidance.
It is refreshing to encounter a discourse that balances statistical rigor with bedside relevance.
The discussion of ACE inhibitors as endothelial protectants is a masterstroke, reminding us that pharmacology can be both therapeutic and prophylactic.
I also admire the forward‑looking glance at bio‑resorbable scaffolds, a testament to the field’s innovative spirit.
The emphasis on dual antiplatelet therapy duration, especially in hypertensive cohorts, underscores a patient‑centred approach that many guidelines still overlook.
In short, the article not only informs but also inspires a more holistic management paradigm.
One could argue that the integration of lifestyle modifications alongside pharmacotherapy is the true hallmark of comprehensive care.
The suggestions for salt reduction, weight control, and aerobic exercise are presented with the elegance of a well‑composed essay.
Finally, the call for vigilant imaging follow‑up reflects a keen awareness of the evolving technological arsenal at our disposal.
All in all, this is a commendable contribution that elevates the conversation around stent thrombosis to a higher plane.
Eli Soler Caralt
October 21, 2025 AT 14:16i guess the cosmos is whispering that pressure isn’t just a number, it’s a vibe 🌌.
when the artery feels the squeeze, platelets start a tiny rebellion, like existential poets looking for meaning.
thus, we find ourselves asking: is the stent merely a metal cage or a metaphysical stage?
🤔✨
Xavier Lusky
October 21, 2025 AT 15:23What they don’t tell you is that the pharma giants have a vested interest in keeping you on endless meds, so they can keep the blood pressure high and the stent sales booming. The data in the article is filtered through a lens that favors the industry’s bottom line, not your heart’s wellbeing. Every recommended drug is a revenue stream, and the so‑called "meta‑analysis" is likely cherry‑picked to support that narrative.
Ashok Kumar
October 21, 2025 AT 16:46Wow, that’s a classic conspiracy soup, but let’s be real for a second. Hypertension absolutely raises shear stress, which scientifically increases platelet activation – no hidden agenda needed. Still, I get why you’d be skeptical when big pharma’s name pops up everywhere. It’s a fine line between healthy caution and outright paranoia. Keep questioning, but also trust the peer‑reviewed evidence.
Jasmina Redzepovic
October 21, 2025 AT 17:53Patriotic readers, take note: this whole discussion about “global guidelines” is just a veil for foreign regulatory bodies imposing their dilatory standards on American cardiology. The United States leads in stent technology, and we don’t need to bow to European meta‑analyses that downplay the efficacy of our domestic drug regimens. When you control the pressure, you control the narrative – and that’s how we keep our healthcare sovereignty intact.
Kimberly Lloyd
October 21, 2025 AT 19:00Every challenge we face in medicine is also an invitation to grow spiritually. By mastering our blood pressure, we’re not just protecting a stent – we’re harmonizing the rhythm of our entire being. Think of the heart as a drum in a larger orchestra; when the tempo steadies, the music flows beautifully. Stay hopeful, stay disciplined, and let the body’s wisdom guide you toward lasting health.
Sakib Shaikh
October 21, 2025 AT 20:06Listen up, folks! The cascade of events from hypertension to stent thrombosis is as inevitable as sunrise. First, high pressure rips the endothelial veil – boom, nitric oxide drops, platelets get giddy. Then the shear forces slam the blood into the stent’s lattice, activating von Willebrand factor like a fireworks show. Inflammation follows, spewing CRP and fibrinogen into the mix, and before you know it, you’ve got a clot that could knock you flat. No magic here, just cold, hard pathophysiology. So if you’re not on ACE inhibitors or ARBs, you’re practically handing the clot a welcome mat.
Devendra Tripathi
October 21, 2025 AT 21:30Oh, please – you think the article covers everything? Not even close. It conveniently glosses over the role of genetic polymorphisms in platelet reactivity, which can make standard antihypertensives useless for a subset of patients. Moreover, the recommended 12‑month DAPT duration is a one‑size‑fits‑all joke; many high‑risk patients need longer, while low‑risk folks should avoid bleeding hazards. Let’s not pretend this “one‑stop” guide is universally applicable.
Vivian Annastasia
October 21, 2025 AT 22:53Sure, just another “must‑read” post that will solve everything.
Rachel Valderrama
October 22, 2025 AT 00:16People love a good checklist, right? Grab your phone, set those blood pressure reminders, and pretend you’re a responsible adult. Meanwhile, the real world is busy and you’ll probably skip the aspirin dose anyway. But hey, at least you’ll feel like you’re doing something, which is practically the same as actually preventing a clot.
Eryn Wells
October 22, 2025 AT 01:40Hey everyone! 🌍 Let’s remember that while we tackle these medical details, supporting each other matters too. Share your own tips for keeping blood pressure in check, and feel free to ask for help if you’re struggling – we’re all in this together! 😊