When you have diabetes, your body struggles to manage blood sugar. Over time, that extra sugar doesn’t just affect your energy or weight-it quietly damages the tiny blood vessels in your eyes. This is diabetic retinopathy, and it’s the leading cause of vision loss in working-age adults in the U.S. The scary part? You might not notice anything wrong until it’s too late.
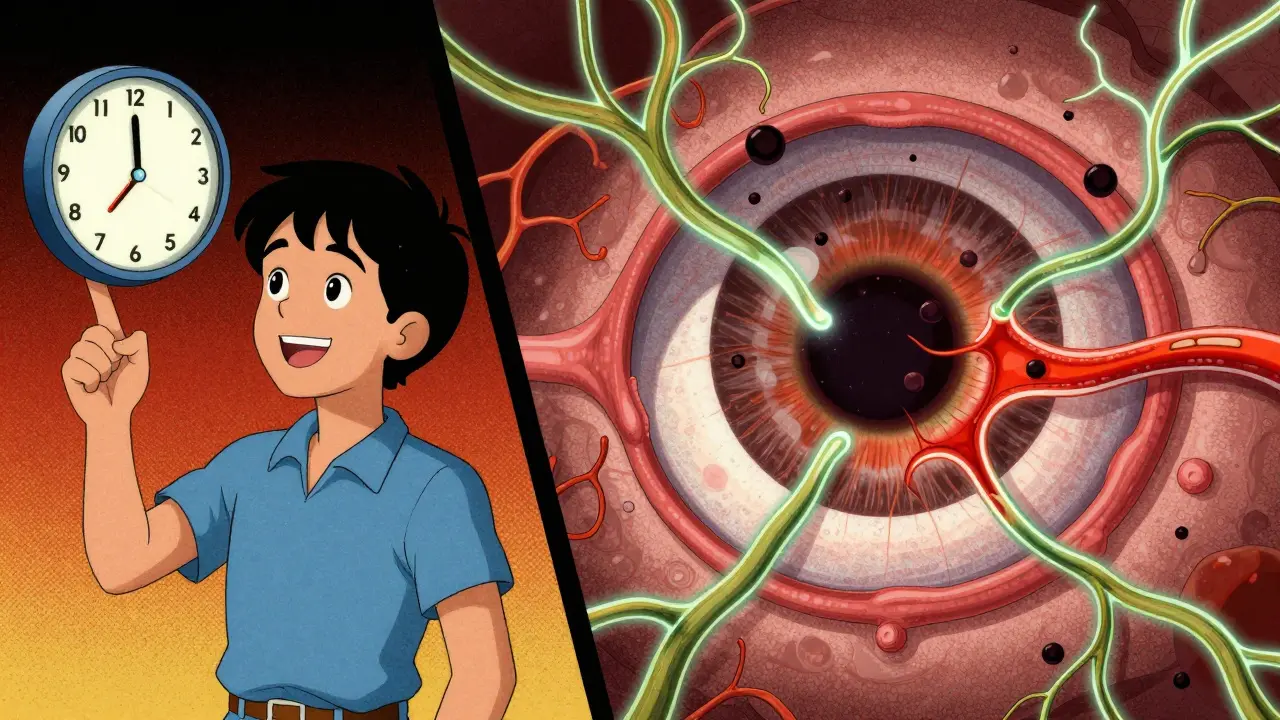
What Happens Inside Your Eye?
Your retina is like the film in a camera. It captures light and sends images to your brain. Behind it are hundreds of tiny blood vessels that feed it oxygen and nutrients. When blood sugar stays high for years, those vessels get damaged. They weaken, leak fluid, or even block off completely. The eye tries to fix this by growing new blood vessels-but they’re messy, fragile, and don’t work right. These abnormal vessels can bleed into the gel-like fluid inside your eye, blur your vision, or even pull the retina away from the back of your eye. That’s called retinal detachment, and it can lead to permanent blindness.Diabetic retinopathy doesn’t happen overnight. It moves in stages:
- Mild nonproliferative: Small bulges called microaneurysms form in vessel walls. You won’t feel anything.
- Moderate to severe nonproliferative: More vessels get blocked. Fluid leaks into the retina, causing swelling-especially in the macula (the center of your vision). This is called diabetic macular edema, and it makes things look blurry or wavy.
- Proliferative: The eye grows new, weak blood vessels on the surface of the retina. These can bleed, scar, and pull the retina loose. This stage is where vision loss becomes serious-and fast.
Diabetic macular edema (DME) happens in about 1 in 15 people with diabetes. It’s not just a side effect-it’s the main reason people with diabetes lose their ability to read, drive, or recognize faces.
Why You Might Not Know You Have It
Most people with early diabetic retinopathy feel fine. No pain. No blurriness. No floaters. That’s why waiting for symptoms is dangerous. By the time you notice dark spots, blurry vision, or trouble seeing at night, the damage is already advanced. Studies show that nearly 70% of patients only realize they have retinopathy when it’s already moderate or worse. That’s why screening isn’t optional-it’s your first line of defense.Here’s what symptoms look like when they finally show up:
- Floaters or dark spots floating across your vision (65% of patients report this)
- Blurred or wavy vision (78% in later stages)
- Difficulty seeing in low light or while driving at night (52%)
- Fading or washed-out colors (41%)
- Loss of side vision (37%)
- Sudden vision loss from bleeding inside the eye
If you’ve had diabetes for more than 10 years, your risk jumps significantly. But even people with Type 2 diabetes who were recently diagnosed can develop retinopathy if their blood sugar isn’t controlled.
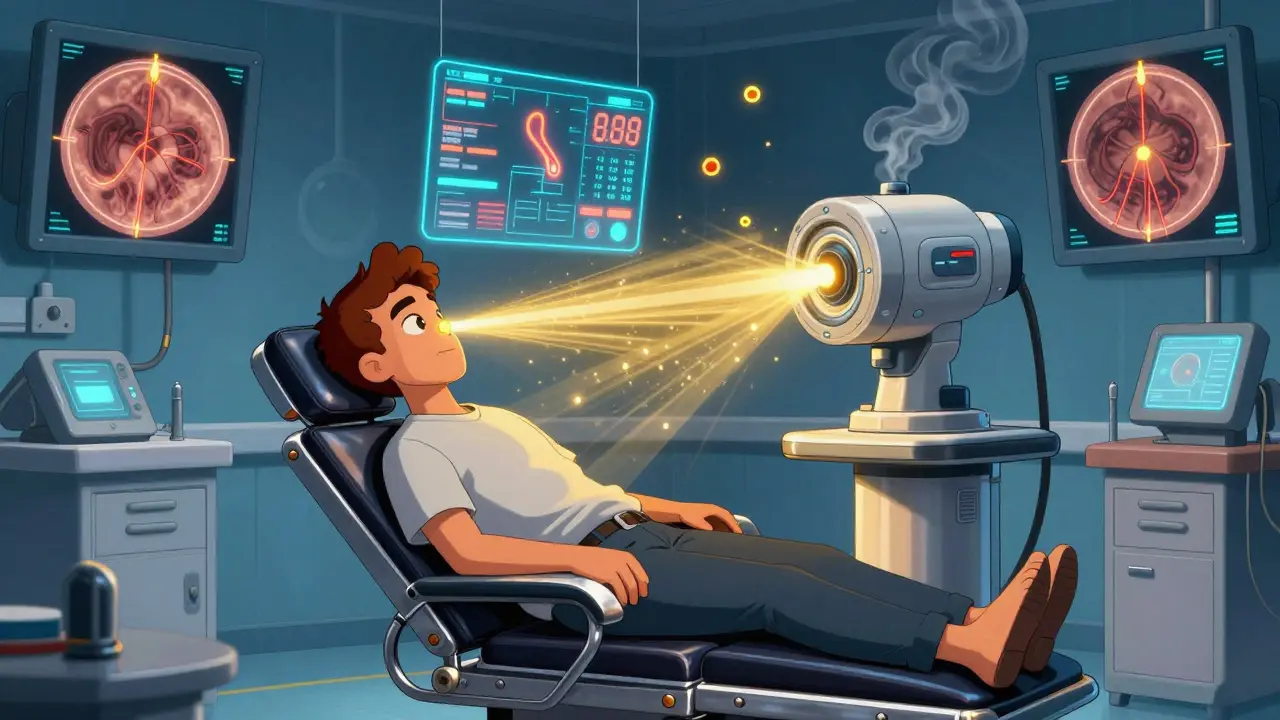
Laser Treatment: How It Stops the Damage
Laser treatment has been the go-to option for decades. It’s not a cure, but it’s one of the most effective ways to stop vision loss. The procedure, called photocoagulation, uses focused beams of light to seal leaking blood vessels or shrink abnormal new ones.There are two main types:
- Focal laser: Used for diabetic macular edema. The doctor targets specific leaky vessels in the macula to stop fluid buildup. This can stabilize vision and sometimes even improve it slightly.
- Scatter laser (panretinal photocoagulation): Used for proliferative retinopathy. Instead of one spot, the laser creates hundreds of tiny burns across the peripheral retina. This doesn’t restore vision, but it cuts off signals that tell the eye to grow new, dangerous blood vessels. The goal? To prevent bleeding and retinal detachment.
The procedure is done in an outpatient clinic. You’ll get numbing drops, and you’ll feel pressure but little to no pain. It usually takes 20 to 30 minutes per eye. You might need more than one session. Afterward, your vision might be blurry for a few hours, and you’ll need someone to drive you home. Some people notice dimmer side vision or trouble seeing in the dark afterward-but that’s a trade-off for keeping central vision.
Studies show that if you get laser treatment before major damage occurs, you have a 95% chance of keeping your vision. That’s not a guarantee, but it’s one of the best odds in medicine.
What Else Helps? Blood Sugar, Blood Pressure, and More
Laser treatment works best when it’s part of a bigger plan. You can’t fix your eyes if your blood sugar is still out of control. Research clearly links high HbA1c levels (a measure of long-term blood sugar) to faster retinopathy progression. Keeping your HbA1c below 7% slows damage. Lower is better-but avoid crashing your sugar. Stability matters more than perfection.High blood pressure and high cholesterol make things worse. They strain the already damaged vessels in your retina. If you have diabetes, aim for:
- Blood pressure under 130/80 mm Hg
- LDL cholesterol under 100 mg/dL
Smoking? Quit. It doubles your risk of retinopathy. Pregnancy? Get checked more often-hormonal changes can speed up damage. And don’t skip your eye exams.
Screening: The Only Way to Catch It Early
The NHS and the American Diabetes Association both recommend a comprehensive dilated eye exam at least once a year. If you already have retinopathy, you might need exams every few months. Don’t wait for symptoms. Don’t assume your vision is fine because you can still read the clock. The damage happens silently.Many clinics now use digital retinal imaging. You look into a camera, and a photo of your retina is taken in seconds. No drops. No pain. No waiting. AI tools can even spot early signs of damage before a doctor does. It’s fast, accurate, and increasingly common-even in rural areas.
What’s Next? New Treatments on the Horizon
Laser treatment isn’t the only tool anymore. Anti-VEGF injections are becoming more common. These are shots into the eye that block a protein (VEGF) that tells the body to grow leaky blood vessels. They’re especially helpful for diabetic macular edema and can improve vision in some cases. They’re not a replacement for laser-they’re often used together.Researchers are also testing new drugs that reduce inflammation in the retina and even gene therapies that could repair damaged blood vessels. But for now, laser treatment, blood sugar control, and regular screenings remain the foundation of care.
What Happens If You Do Nothing?
Without treatment, diabetic retinopathy can lead to:- Permanent vision loss
- Blindness
- Retinal detachment requiring emergency surgery
- Neovascular glaucoma-a painful form of glaucoma caused by abnormal blood vessels blocking fluid drainage
It’s not inevitable. But it’s silent. And it’s progressive. The longer you wait, the less treatment can do.
Can diabetic retinopathy be reversed?
Early damage can be stopped or slowed, but once photoreceptor cells in the retina die, the vision loss is permanent. That’s why catching it early is everything. Laser and injections can prevent further harm, but they won’t bring back vision you’ve already lost.
Do I still need laser treatment if I’m on insulin?
Yes. Insulin helps control blood sugar, but it doesn’t undo damage already done to your eyes. Laser treatment is based on the condition of your retina-not your diabetes medication. Even people on insulin can develop retinopathy if their sugar levels have been high in the past.
How often should I get my eyes checked if I have Type 2 diabetes?
At least once a year. If you have no signs of retinopathy, yearly exams are usually enough. If you have early changes, your eye doctor may suggest exams every 6 to 9 months. If you’re pregnant or have advanced retinopathy, you might need monthly checks.
Is laser treatment painful?
Most people feel pressure or a slight pinch, but not pain. Numbing drops are used, and the procedure is quick. Some people get mild headaches or blurry vision afterward, but it usually clears up in a few hours. Severe pain is rare and should be reported immediately.
Can I drive after laser treatment?
Not right away. Your pupils will be dilated, and your vision might be blurry for several hours. You’ll need someone to drive you home. Avoid driving until your vision is clear and stable.
Final Thought: Your Eyes Don’t Lie
You can ignore your blood sugar numbers. You can skip your gym sessions. But your eyes? They remember everything. Every spike, every long night of high sugar, every missed checkup-it all adds up. Diabetic retinopathy doesn’t care how young you are or how healthy you feel. It only cares about time and control.Get your eyes checked. Keep your sugar steady. Don’t wait for the floaters. Because when it comes to your vision, the best treatment is the one you do before you even know you need it.






Irish Council
February 19, 2026 AT 12:31Laser treatment? More like government-funded eye torture. They don't tell you the laser burns holes in your retina permanently. Next they'll say it's for your own good.
I read a study once - 40% of people who got laser ended up with night blindness. No one talks about that.
Big Pharma loves this. They don't want you cured. They want you coming back for more shots and more lasers.
Ever wonder why they never mention fasting or magnesium? Nah. Too cheap. Too real.