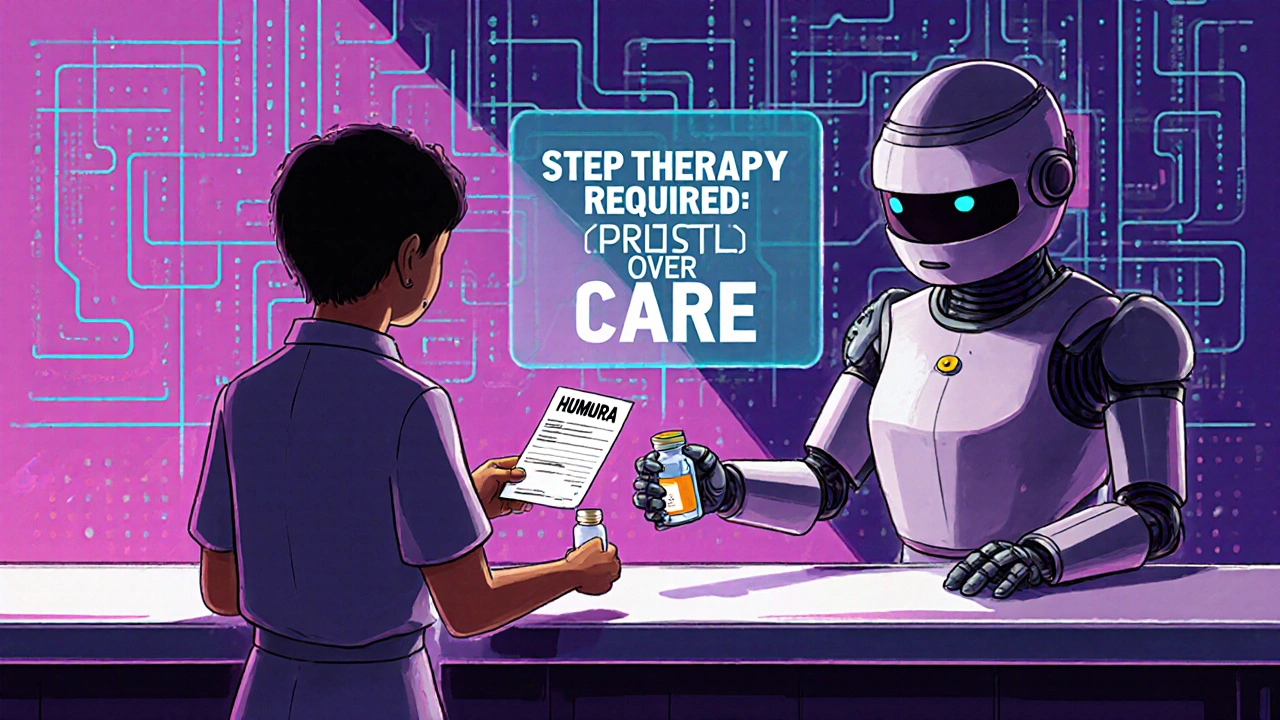
Step Therapy Exception: When Insurance Denies Your Medication and How to Fight Back
When your doctor prescribes a medication that works for you, but your insurance forces you to try cheaper options first—that’s step therapy, a cost-control practice where insurers require patients to try lower-cost drugs before approving the prescribed one. Also known as fail first, it’s common in Medicare, Medicaid, and private plans. But if those cheaper drugs won’t work for you—or already failed—there’s a way out: a step therapy exception, a formal request to bypass the required drug trials and get coverage for the medication your doctor actually recommended.
This isn’t just paperwork. It’s a lifeline for people with chronic conditions like rheumatoid arthritis, multiple sclerosis, or depression, where the wrong drug can cause serious harm or delay recovery. For example, if you’ve already tried two generic antidepressants that made you dizzy or nauseous, your doctor can argue that forcing you to try a third is unsafe. The same goes for biologics used in autoimmune diseases—those aren’t interchangeable with cheap pills, and insurers know it. But they still make you ask. A step therapy exception, a formal request to bypass the required drug trials and get coverage for the medication your doctor actually recommended. requires a letter from your provider explaining why the preferred drugs won’t work, won’t be tolerated, or have already failed. Some plans require lab results, prior treatment records, or even a phone call from your doctor. The key is documentation. Without it, your request gets denied. And if you’re denied, you can appeal. Many patients don’t know this, but over 70% of step therapy exceptions are approved when properly supported.
You’ll find real examples in the posts below—like how patients fought to get access to branded drugs after generics caused side effects, or how people with nerve pain skipped ineffective medications to get pregabalin covered. Others show how biosimilar substitution rules can clash with step therapy, or how food allergies complicate treatment paths that ignore individual biology. These aren’t theoretical stories. They’re from people who pushed back, filed appeals, and got the meds they needed. If you’re stuck in a cycle of failed trials, this collection gives you the exact steps to take, the language to use, and the evidence to back it up. No fluff. Just what works.
 20 November 2025
20 November 2025
How to Appeal Insurance Denials for Generic Medications: A Step-by-Step Guide
Learn how to successfully appeal your insurance denial for generic medications with a step-by-step guide backed by real data, doctor tips, and proven strategies to get your prescribed drug covered.
Latest Posts
-

Medication List Templates: Free Printable and Digital Options for 2026
-

PrescriptionPoint Online Pharmacy: Safe, Affordable Medication Delivered
-
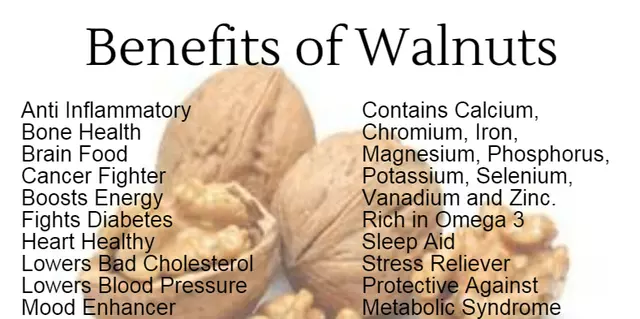
Boost Your Immunity and Revitalize Your Body with the Amazing Benefits of Danshen
-
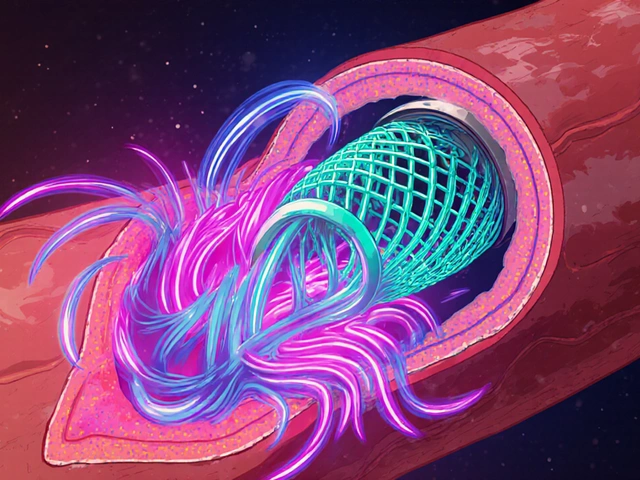
How High Blood Pressure Increases Risk of Blood Clots in Stents
-

Buy Generic Crestor (Rosuvastatin) Online Cheap: Safe 2025 Prices, Rx Rules, and Smarter Options

11