Sleep Therapy for PTSD: What Works and What to Avoid
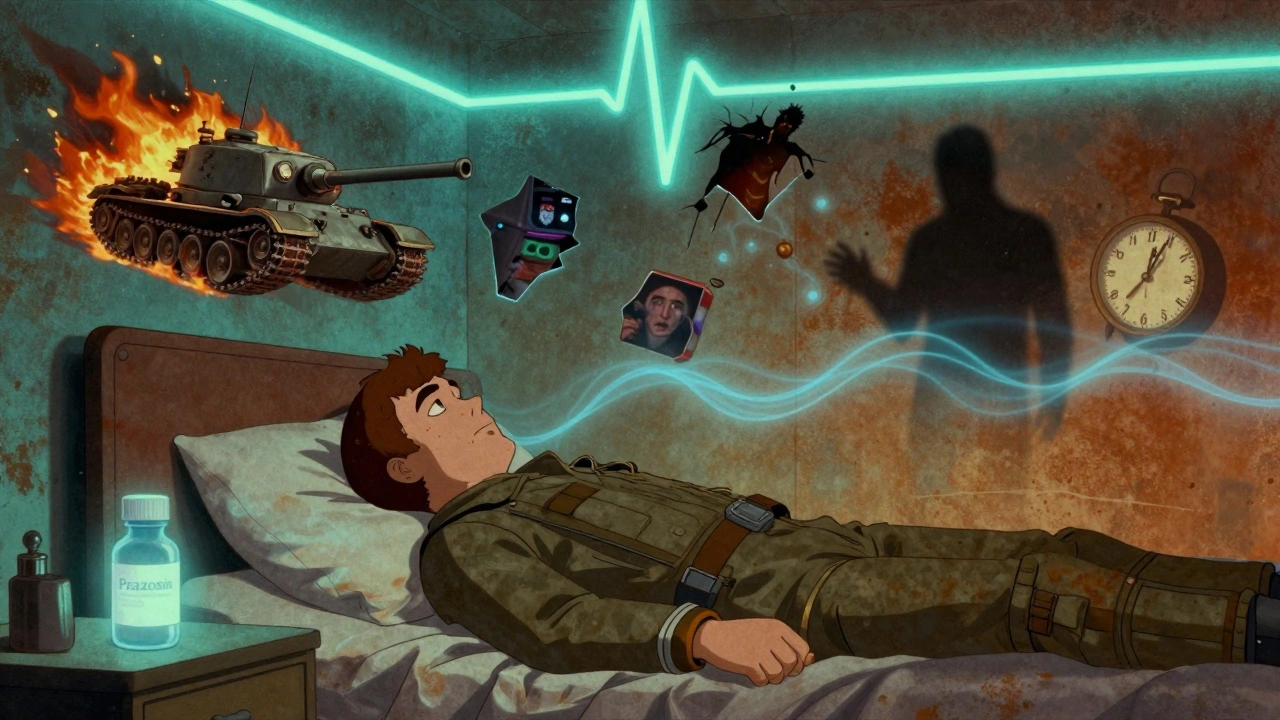
When sleep therapy for PTSD, a targeted approach to fixing trauma-driven insomnia by rewiring how the brain processes fear during sleep. Also known as trauma-focused sleep intervention, it’s not just about sleeping longer—it’s about stopping nightmares, reducing hypervigilance, and breaking the cycle where trauma steals your rest and restlessness fuels your symptoms. If you’ve tried sleeping pills, meditation apps, or just "trying harder" to relax at night, you know they often fall short. That’s because PTSD doesn’t just keep you awake—it rewires your nervous system to stay on high alert, even when your body is exhausted.
The biggest problem? Most people assume sleep issues from PTSD are just stress-related. But research shows trauma survivors often develop a unique type of insomnia where the brain treats sleep like a threat. Nightmares aren’t just bad dreams—they’re replay loops of the trauma, triggered by REM sleep. And when you start avoiding sleep to dodge them, your body never gets the deep rest it needs to heal. That’s where CBT-I for PTSD, a modified form of cognitive behavioral therapy designed specifically to treat trauma-related sleep problems comes in. Unlike general sleep hygiene advice, CBT-I for PTSD combines exposure techniques, imagery rehearsal, and sleep restriction to directly target the fear-response loop. It’s not magic, but it’s proven: studies show over 60% of patients report fewer nightmares and better sleep after 6–8 weeks.
Another key player is trauma-related insomnia, a clinical subtype of insomnia caused by persistent trauma memories disrupting sleep architecture. It’s different from regular insomnia because it’s tied to flashbacks, startle responses, and a constant sense of danger—even in a safe room. This is why simply cutting caffeine or turning off screens won’t fix it. You need to retrain your brain’s threat detection system while you’re asleep. That’s why therapies like imagery rehearsal therapy (IRT), where you rewrite the ending of your nightmare while awake, work so well. It’s not about forgetting the trauma—it’s about changing how your brain handles it at night.
What doesn’t work? Sleeping pills. Benzodiazepines and sleep aids might help you nod off, but they don’t touch the root cause—and they can make nightmares worse over time. Even melatonin, often recommended for sleep, has little proven effect on PTSD-related nightmares. What does help? Consistent routines, reducing nighttime stimulation, and therapies that address the emotional weight of the trauma while you’re still awake. And yes, it takes time. But if you’ve been stuck in this loop for months or years, you’re not broken—you’re just missing the right tool.
Below, you’ll find real-world guides on how to track your progress, what medications can help or hurt, how to spot when therapy is working, and why some common advice actually makes things worse. These aren’t theoretical tips—they’re from people who’ve been there and found what actually moves the needle.
 1 December 2025
1 December 2025
PTSD Nightmares: How Prazosin and Sleep Therapies Really Work
PTSD nightmares are common and debilitating. Learn how prazosin and sleep therapies like CBT-I and IRT work, what the research says, and which options actually lead to lasting recovery.
Latest Posts
-
Boost Your Immunity and Revitalize Your Body with the Amazing Benefits of Danshen
-

How sorafenib is improving the prognosis of advanced cancer patients
-

Explore 5 Alternatives to Cialis for Effective ED Management
-

Authorized Generic Pricing: Why They Cost Less Than Brand Name Drugs
-

Boost Your Overall Health with the Power of Fructo-Oligosaccharides Dietary Supplement

15