For many people living with PTSD, the worst part isn’t the memories-it’s what happens when they close their eyes. Nightmares don’t just disrupt sleep; they keep trauma alive. Studies show 71% to 90% of military veterans with PTSD and over half of civilian survivors experience frequent, terrifying nightmares that feel real. These aren’t ordinary bad dreams. They replay trauma with brutal detail, often leaving people exhausted, anxious, and afraid to sleep. And while trauma-focused therapy is the gold standard for PTSD, nightmares often stick around even after other symptoms improve. That’s where treatments like prazosin and sleep-focused therapies come in.
What Prazosin Does (and Doesn’t Do)
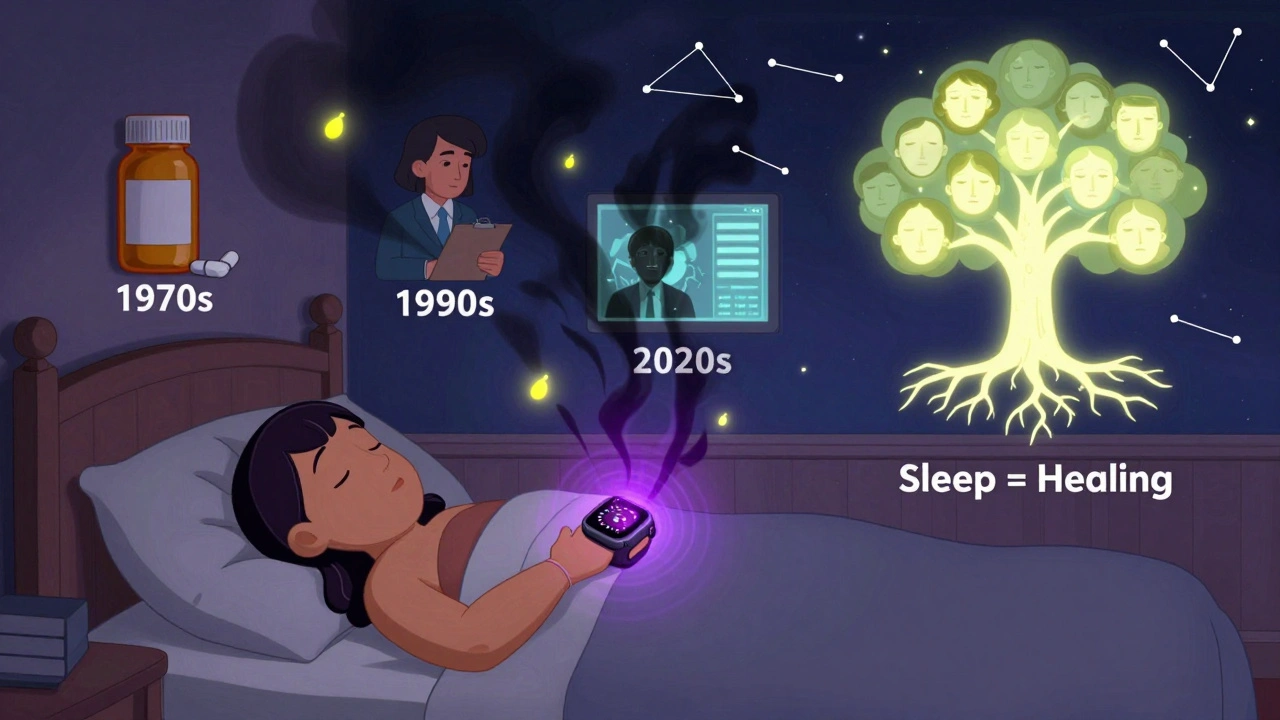
Prazosin was never meant to treat PTSD. It was developed in the 1970s as a blood pressure medication. But in 2003, a VA doctor named Dr. Murray Raskind noticed something strange: veterans taking prazosin for hypertension were sleeping better and having fewer nightmares. That accidental discovery changed the course of PTSD treatment.
Today, prazosin is used off-label for PTSD nightmares. It works by blocking alpha-1 receptors in the brain, which reduces the surge of adrenaline that fuels nightmares during REM sleep. Most people take 1-25 mg at night, usually starting low-1 mg-and slowly increasing until the nightmares ease or side effects appear. The goal is usually 3-15 mg, taken 60-90 minutes before bed to match peak blood levels.
But here’s the catch: prazosin doesn’t cure PTSD. It doesn’t erase trauma. It just quiets the nighttime chaos. A 2022 meta-analysis found it reduces nightmare frequency with a moderate effect size-but has almost no impact on overall PTSD symptoms like flashbacks, avoidance, or hypervigilance. That means it’s not a standalone solution. It’s a tool for sleep, not healing.
Side effects are real. About 44% of users report dizziness, especially when standing up fast. Nasal congestion and low blood pressure are common too. Some people stop taking it because they feel lightheaded. And if you quit suddenly? Around 28% experience rebound nightmares-worse than before. That’s why tapering off slowly under medical supervision is critical.
Why Sleep Therapies Are More Powerful Than You Think
If prazosin silences the noise, sleep-focused therapies like CBT-I and IRT actually rewire the brain’s response to trauma. And they work better in the long run.
Cognitive Behavioral Therapy for Insomnia (CBT-I) is the most studied and recommended sleep treatment for PTSD. It’s not just about sleeping more-it’s about fixing broken sleep habits. A typical CBT-I program lasts 6-8 weeks and includes:
- Stimulus control: Get out of bed if you’re awake for more than 20 minutes. Only return when sleepy.
- Sleep restriction: Limit time in bed to match actual sleep time (e.g., if you only sleep 5 hours, you get 5 hours in bed-even if you’re tired).
- Cognitive restructuring: Challenge thoughts like “I’ll never sleep again” or “If I don’t sleep, I’ll break down.”
- Sleep hygiene: No screens before bed, consistent schedule, cool dark room.
- Relaxation training: Breathing, muscle relaxation, mindfulness.
Studies show CBT-I reduces insomnia severity by a large margin-far more than any medication. In one VA study, patients who did CBT-I along with prolonged exposure therapy improved their sleep efficiency by 15.3%, added 78 minutes of sleep per night, and slashed their insomnia scores by 12.4 points. That’s more than double the gains from medication alone.
And here’s something surprising: CBT-I also reduces PTSD symptoms. Why? Because sleep isn’t just a symptom-it’s a recovery pathway. When you sleep better, your brain processes fear more effectively. Brain scans show the amygdala (the fear center) calms down after CBT-I. Emotional regulation improves. People feel less overwhelmed during the day.

Imagery Rehearsal Therapy: Rewriting Your Nightmares
Imagery Rehearsal Therapy (IRT) is like mental rehearsal-but for nightmares. You pick a recurring nightmare, write down the script, then rewrite it into a new, positive or neutral version. You rehearse this new version for 10-20 minutes every day while awake.
It sounds simple. But it’s powerful. In studies, 67-90% of PTSD patients report fewer nightmares after just 3-5 sessions. One veteran described it as “taking back control.” Instead of being trapped in the trauma, he became the author of his dreams. He changed a nightmare of being chased into one where he stood tall, turned around, and walked away.
Unlike prazosin, IRT doesn’t rely on chemicals. It doesn’t cause dizziness or low blood pressure. It requires effort-but it builds resilience. The National Center for PTSD found 85% of users felt less distress from nightmares after IRT. And the gains last. People who stick with it report fewer nightmares even a year later.
The Real Problem: Access and Misconceptions
Here’s the uncomfortable truth: most people with PTSD nightmares never get these treatments. In VA systems, 78% of veterans get medication like prazosin. Only 32% get evidence-based therapy like CBT-I or IRT.
Why? Access. CBT-I requires trained therapists. There are only 412 certified CBT-I providers nationwide. Insurance often limits sessions to 6, even though 8 are proven to work. Rural veterans face 47% lower access than those in cities. Many clinicians don’t feel trained to handle trauma-related sleep issues. And patients? They’re afraid.
“I don’t want to talk about the trauma again,” one patient told a VA therapist. “I just want to sleep.” That’s understandable. But here’s the twist: you don’t need to relive the trauma in CBT-I or IRT. These therapies focus on sleep, not memory. You don’t have to describe the nightmare in detail. You just need to rewrite it-or change your relationship to sleep.
Another myth: “Prazosin is easier.” Maybe. But it’s temporary. If you stop, nightmares often return. CBT-I and IRT teach skills that last. They’re like learning to swim-you don’t need a life jacket forever.
What Works Best Together
The strongest evidence points to combining treatments. CBT-I paired with Prolonged Exposure therapy (CBT-I-PE) outperforms either alone. People sleep longer, feel calmer, and recover faster. The VA now calls this “integrated sleep-PTSD treatment.”
And new tools are emerging. The NightWare app, FDA-approved in 2020, uses an Apple Watch to detect signs of a nightmare-increased heart rate, movement-and sends gentle vibrations to disrupt REM sleep without waking the person. In trials, it cut nightmares by 58%. It’s not a cure, but it’s a bridge for people who can’t access therapy.
For those who can’t tolerate prazosin, or can’t find a therapist, NightWare, IRT, or even brief behavioral treatments (BBTI) can be a start. BBTI is a 4-session version of CBT-I. In VA trials, 83% of patients responded to it. It’s short, structured, and doesn’t require a specialist.
What to Do Next
If you or someone you know struggles with PTSD nightmares, here’s what to try:
- Track your nightmares. Write down what happens, how often, and how you feel after. Even 2 weeks of notes helps.
- Ask your doctor about prazosin. If you’re considering it, start low (1 mg), monitor blood pressure, and don’t stop suddenly.
- Request CBT-I or IRT. Tell your provider you want sleep-focused therapy, not just pills. Ask if they offer it-or can refer you.
- Try the CBT-I Coach app. Free through the VA. Guides you through core techniques with daily exercises.
- Consider NightWare. If you have an Apple Watch, it’s an FDA-cleared option for nightmare reduction.
There’s no magic bullet. But there is hope. You don’t have to live with terror every night. Sleep isn’t just rest-it’s repair. And with the right tools, your brain can heal-even after trauma.
Does prazosin cure PTSD nightmares?
No, prazosin doesn’t cure PTSD. It reduces nightmare frequency and intensity by blocking adrenaline surges during sleep. It’s a symptom management tool, not a treatment for trauma itself. Symptoms often return if you stop taking it.
Is CBT-I better than prazosin for PTSD nightmares?
Yes, for most people. CBT-I has stronger, longer-lasting effects on both sleep and PTSD symptoms. It improves sleep efficiency, reduces insomnia severity, and helps regulate emotions. Prazosin helps with nightmares but doesn’t improve overall PTSD. CBT-I teaches skills that last; prazosin only works while you’re taking it.
Can I use prazosin and CBT-I together?
Yes, and many experts recommend it. Prazosin can help stabilize sleep enough to start therapy. Once CBT-I takes effect, some people reduce or stop prazosin. Combining both often leads to faster and more complete recovery than either alone.
Why isn’t prazosin FDA-approved for PTSD nightmares?
The FDA rejected prazosin’s application in 2021 because clinical trials showed inconsistent results. Some studies found big benefits; others found little to no difference from placebo. Experts believe this is due to poor dosing, short treatment lengths, or including patients without severe nightmares. It’s still widely used off-label because many patients benefit.
How long does it take for CBT-I to work for PTSD nightmares?
Most people see improvements in 4-6 weeks. The first few weeks can be hard-sleep restriction makes you tired. But by week 6, sleep efficiency and nightmare frequency usually drop significantly. Long-term gains are maintained at 6-month and 1-year follow-ups.
Are there side effects to CBT-I or IRT?
The main side effect is temporary sleep disruption during the first week or two of sleep restriction. Some people feel exhausted or irritable. But these effects fade as sleep improves. Unlike medication, there are no physical side effects like dizziness or low blood pressure. The biggest challenge is sticking with it-especially if you’re dealing with trauma.
Can shift workers use CBT-I for PTSD nightmares?
Yes, but it’s harder. CBT-I relies on consistent sleep schedules, which shift work disrupts. Clinicians can adapt protocols-for example, using sleep restriction within a worker’s shift cycle instead of a fixed bedtime. Digital tools like the CBT-I Coach app help track sleep patterns even with irregular hours. Success is possible but requires more flexibility and support.
What’s the most effective treatment for PTSD nightmares right now?
The most effective approach is a combination: trauma-focused therapy (like CPT or PE) for the root cause, plus CBT-I or IRT for persistent nightmares. For those who can’t access therapy, prazosin or NightWare can help manage symptoms. But long-term recovery comes from rebuilding sleep and emotional regulation-not just suppressing nightmares.





alaa ismail
December 2, 2025 AT 08:41Been on prazosin for 8 months. Sleep’s way better, but I still wake up sweating sometimes. It’s not magic, but it’s the only thing that lets me close my eyes without bracing for the nightmare.
ruiqing Jane
December 3, 2025 AT 08:57I’m so tired of people treating meds like the enemy. Prazosin didn’t ‘fail’ me-it gave me the breathing room to even start therapy. I did IRT after 3 months. Now I dream about hiking. Real hiking. Not running from shadows.
Fern Marder
December 4, 2025 AT 22:34CBT-I is just sleep hygiene with a fancy name 😒. And don’t get me started on ‘rewriting nightmares’-like, you think your brain’s gonna listen to you because you wrote a happy ending? 🤦♀️
Allan maniero
December 5, 2025 AT 07:27It’s fascinating how the medical establishment latches onto pharmacological solutions before investing in behavioral ones. Prazosin is convenient, yes-but it’s also a band-aid on a hemorrhage. The brain isn’t a circuit board you can tweak with alpha-blockers; it’s a narrative engine. When trauma becomes a looping script, the solution isn’t to mute the volume-it’s to rewrite the screenplay. That’s what IRT does. It’s not therapy. It’s authorship.
Paul Santos
December 5, 2025 AT 17:48Let’s be real-prazosin’s just a glorified alpha-blocker that got lucky in a VA study. The real breakthrough? The fact that the VA still hasn’t trained 10% of its clinicians in IRT. We’re treating symptoms like they’re the disease. Classic biomedical reductionism. 😴
Doug Hawk
December 6, 2025 AT 03:22so i tried prazosin and it made me dizzy like whoa and then i stopped and had like 3 nights of nightmares that felt like my brain was being rewired by demons idk
Kristen Yates
December 7, 2025 AT 15:35I used to think sleep was just rest. Now I know it’s the only time my brain tries to heal itself. If nightmares steal that, they steal recovery. IRT gave me back my dreams. Not the ones I wanted-but the ones I could survive.
Saurabh Tiwari
December 8, 2025 AT 01:44bro i tried nightware on my apple watch and it vibed me awake like 3 times a night and i was so tired i just uninstalled it lmao
Michael Campbell
December 9, 2025 AT 19:03Why does the VA push this stuff? It’s all part of the mental health industrial complex. They don’t want you healed-they want you medicated and quiet. Prazosin keeps you docile. Therapy? That’s dangerous. It makes you remember.
Victoria Graci
December 11, 2025 AT 10:39There’s something profoundly human about reclaiming your dreams. We don’t just want to sleep-we want to imagine. Trauma steals the future from your unconscious. IRT doesn’t just change the dream-it restores your right to dream at all. That’s not therapy. That’s resurrection.
Carolyn Woodard
December 12, 2025 AT 22:11It’s interesting how CBT-I’s efficacy correlates with amygdala downregulation. The neuroplasticity involved in sleep restructuring suggests that the limbic system can be retrained without direct trauma exposure. This challenges the assumption that reprocessing memories is necessary for symptom resolution. Sleep as a modulator of fear extinction-fascinating.
Sandi Allen
December 13, 2025 AT 00:05Who funded these studies? Big Pharma? The VA? The government? They’re all lying to you. Prazosin’s side effects are worse than the nightmares. And CBT-I? It’s designed to make you dependent on therapists so they can keep getting paid. Wake up!
John Webber
December 14, 2025 AT 19:48i used to think i was broken but then i did 4 sessions of bbt i and now i sleep 7 hours. no pills. no therapy. just a stupid app. my therapist said i was lucky. i said no. i was smart.
Saravanan Sathyanandha
December 15, 2025 AT 23:01In India, PTSD is still whispered about. We don’t have access to prazosin, let alone IRT. But my cousin, a veteran of the Kargil conflict, started writing his nightmares down-then rewriting them as poems. He didn’t know what IRT was. He just needed to feel like he could end the story. Now he teaches it to others in his village. Sometimes healing doesn’t need a clinic. It just needs a pen.
Shubham Pandey
December 17, 2025 AT 01:50prazosin works. stop overthinking it.