Prior Authorization Appeal: How to Fight Insurance Denials and Get Your Medication Covered
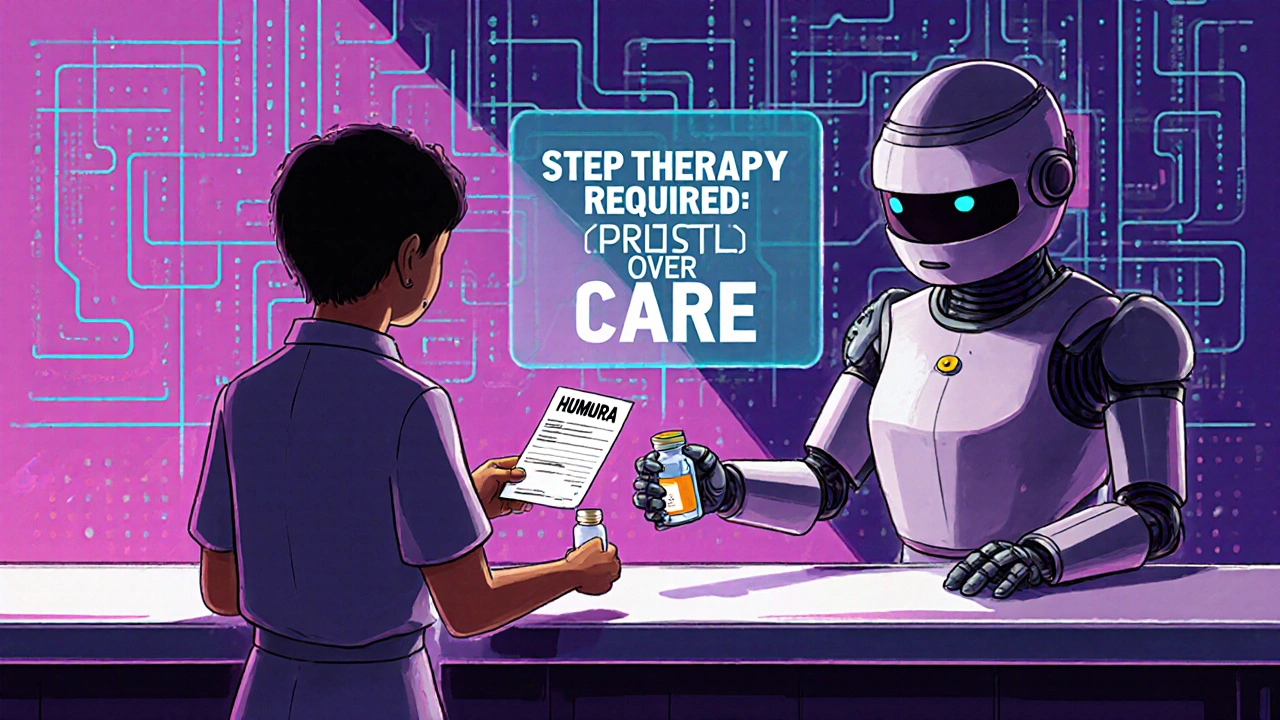
When your doctor prescribes a medication but your insurance says prior authorization, a process where insurers require approval before covering certain drugs. Also known as pre-authorization, it's meant to control costs—but too often, it becomes a roadblock to care. You’re not alone. Millions of patients face this every year, especially for specialty drugs, mental health meds, or newer treatments. The system isn’t broken—it’s just stacked against you unless you know how to push back.
A prior authorization appeal, a formal request to reverse an insurance denial after an initial rejection. Also known as drug coverage appeal, it’s your legal right under federal and state laws. Most denials happen because the insurer thinks a cheaper alternative will work—or because your doctor didn’t fill out the paperwork right. But if the alternative is unsafe, ineffective, or already failed for you, you have strong grounds to appeal. The key isn’t yelling at customer service. It’s using your medical records, your doctor’s letter, and the insurer’s own guidelines to prove why this drug is necessary.
Insurers often deny coverage for drugs like gabapentin, tadalafil, or even common generics if they’re not on their preferred list. But look at the posts here: people are fighting for access to everything from antifungal creams to ADHD meds to blood pressure pills. One person got Ivermectin approved after proving they had a parasitic infection no other drug touched. Another won back coverage for imipramine after showing their depression didn’t respond to SSRIs. These aren’t rare cases—they’re repeatable wins.
You don’t need a lawyer. You don’t need to be rich. You just need to know what to say, what to submit, and when to escalate. The insurance denial, a refusal by a health plan to pay for a prescribed medication or service. Also known as coverage denial, it’s just the first step in a process you can control. Most appeals get approved on the first try if you include: a detailed letter from your provider, copies of failed alternatives, and a clear explanation of why the drug is medically necessary. Some insurers even have online appeal forms—skip the phone calls and go straight to the paperwork.
And if your appeal gets denied? There’s a second layer: external review. State insurance departments can step in. Medicare and Medicaid have their own appeal paths. And if you’re on a private plan, the Affordable Care Act gives you the right to an independent third-party review. This isn’t theoretical—it’s happening every day in doctor’s offices, pharmacies, and patient advocacy groups.
What you’ll find below are real stories from people who’ve been there. They fought for hyperacusis therapy when insurers called it "experimental." They won coverage for biosimilars after being told only the brand name counted. They got their ADHD meds approved after proving the cheaper version caused panic attacks. These aren’t outliers. They’re templates. Every appeal here follows the same structure: document everything, cite the guidelines, and never accept "no" as the final answer.
 20 November 2025
20 November 2025
How to Appeal Insurance Denials for Generic Medications: A Step-by-Step Guide
Learn how to successfully appeal your insurance denial for generic medications with a step-by-step guide backed by real data, doctor tips, and proven strategies to get your prescribed drug covered.
Latest Posts
-

Best CVS Alternatives: Top Pharmacies & Online Prescription Services in 2025
-

Top Alternatives to Northwest Pharmacy: Finding the Best Online Pharmacies in 2024
-

The Crucial Role of Fluconazole in Managing HIV/AIDS
-

Elderly Dehydration and Diuretics: How to Protect Kidneys and Prevent Hospitalization
-

Meniscus and ACL Injuries: Understanding Knee Pain and When Surgery Is Necessary

11