Corticosteroid Psychosis Risk Assessment Tool
Assess Your Risk
This tool estimates your risk of corticosteroid-induced mood changes and psychosis based on factors discussed in the article.
Your Risk Assessment
When you’re prescribed corticosteroids for asthma, rheumatoid arthritis, or a flare-up of an autoimmune condition, you’re usually focused on getting relief from pain, swelling, or breathing trouble. But there’s a side effect many doctors don’t talk about - one that can turn your mood upside down, make you feel like you’re losing your mind, or even trigger full-blown psychosis. It’s not rare. It’s not theoretical. And it’s happening to people right now - including older adults taking daily pills for chronic conditions.
It’s Not Just Feeling ‘On Edge’
Corticosteroids like prednisone, dexamethasone, and methylprednisolone don’t just calm inflammation. They also flood your brain with hormone-like signals that can scramble your mood, thoughts, and behavior. The changes don’t always look like depression or anxiety. Sometimes, they start with feeling unusually happy - euphoric, even - followed by sudden irritability, sleepless nights, or wild mood swings. One patient described it as feeling like ‘someone switched my personality off and on without asking.’Studies show these effects aren’t rare. About 5% to 18% of people taking systemic corticosteroids experience some kind of psychiatric reaction. At doses below 40 mg of prednisone per day, the risk is low - around 1.3%. But push past that threshold, and the risk jumps to nearly 1 in 5. That’s not a fluke. That’s a clear dose-response pattern. The higher the dose, the higher the chance your brain gets caught in the crossfire.
When Does It Start - And How Long Does It Last?
Symptoms don’t wait months to show up. Most people notice something off within the first few days. The median time? Three to four days after starting the medication. Some feel it even sooner - within 48 hours. That’s why confusion, agitation, or sudden insomnia in the first week of treatment should raise a red flag, not get dismissed as ‘stress’ or ‘side effects of being sick.’What’s more alarming? These symptoms don’t always vanish when you stop the drug. Case reports in recent research show that psychosis and mania can persist for weeks - sometimes months - after corticosteroids are fully cleared from the body. This isn’t just withdrawal. It suggests the brain may be rewired temporarily, or even permanently, by the exposure. That’s why stopping the medication isn’t always the end of the story.
Who’s Most at Risk?
It’s not random. Certain people are far more likely to experience these effects. Women are consistently reported to be more vulnerable than men, though the reason isn’t fully understood. Older adults - especially those over 65 - are at higher risk, partly because they often take higher doses for longer periods, and their brains are more sensitive to hormonal shifts.If you already have a psychiatric history - particularly bipolar disorder - your risk skyrockets. One study found that 11.8% of clinical cases involved mania alone, while 23.5% involved psychosis without mania. That means you can develop hallucinations or delusions without ever feeling ‘up’ or hyper. You might just feel paranoid, convinced people are watching you, or hear voices that aren’t there. And if you’re not screened, it’s easy to mistake this for dementia, delirium, or even schizophrenia.

What’s Happening in the Brain?
We don’t have all the answers, but we know enough to see the pattern. Corticosteroids interfere with the hypothalamus-pituitary-adrenal (HPA) axis - your body’s natural stress-response system. When you take synthetic steroids, your brain thinks it’s flooded with cortisol and shuts down its own production. That disruption affects neurotransmitters, especially dopamine. Animal studies show corticosteroids trigger a spike in tyrosine hydroxylase, the enzyme that makes dopamine. Too much dopamine = psychosis.There’s also damage to the hippocampus - the part of your brain responsible for memory and emotional regulation. That’s why many patients report trouble remembering things, feeling mentally foggy, or struggling to focus - even if they’re not psychotic. These cognitive changes often show up before mood swings, making them early warning signs.
How Do Doctors Miss This?
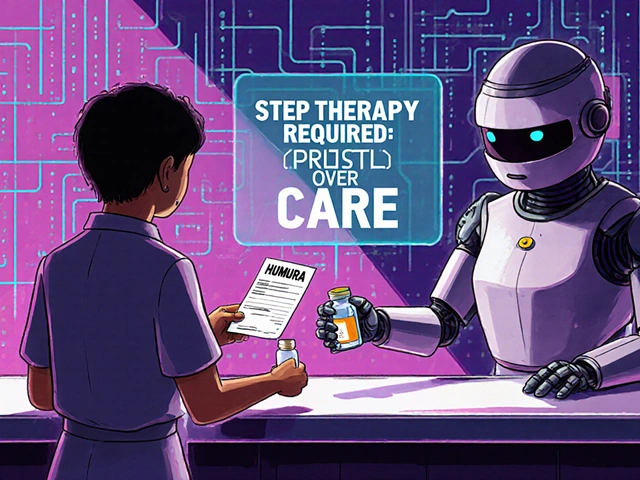
Because the symptoms look like so many other things. Confusion? Could be infection. Mood swings? Could be stress from being sick. Psychosis? Could be schizophrenia. That’s why corticosteroid-induced psychosis is often a diagnosis of exclusion. Doctors have to rule out everything else - metabolic imbalances, drug interactions, brain tumors, infections - before they even consider the steroid as the cause.And here’s the kicker: most prescribing guidelines don’t mention psychiatric screening. Pharmacists know corticosteroids are among the most prescribed drugs worldwide - 10 million new oral prescriptions in the U.S. every year. But only a fraction of patients are warned about mood risks. The FDA hasn’t approved a single drug specifically for treating steroid-induced psychosis. That means doctors are using antipsychotics off-label - haloperidol, olanzapine, risperidone - with varying success.
What Should You Do If You Notice Changes?
If you or someone you care for starts taking corticosteroids and begins to feel ‘not like themselves,’ don’t wait. Track the symptoms. Write them down. Note when they started. Did sleep disappear? Did you become overly suspicious? Did you hear voices? Did you feel like you were on top of the world one day and suicidal the next?Call your doctor immediately. Don’t assume it’s ‘just anxiety.’ Ask: Could this be from the steroid? If the dose is over 40 mg of prednisone per day, tapering it down - even slightly - often brings relief. In fact, 92% of patients see their symptoms improve when the dose is lowered below that threshold.
If stopping or reducing the steroid isn’t possible - say, because you’re fighting a life-threatening flare - then psychiatric help is essential. Low-dose antipsychotics can work fast. Some patients stabilize within days. Lithium has been used to prevent mania, but it’s risky and requires close monitoring. Never try to manage this alone.
What’s Not Being Done - And Why It Matters
We’ve known about this for over 70 years. The first reports came in the late 1940s, right after synthetic steroids hit the market. Yet today, there’s still no standardized tool to screen for these effects. No checklist. No blood test. No easy way for a rheumatologist or pulmonologist to know if their patient is slipping into psychosis.Experts are calling for ‘clinimetric methods’ - simple, quick rating scales that nurses or pharmacists can use during routine check-ins. Imagine a three-question screen: Have you felt unusually high or irritable? Have you had strange thoughts or heard things others don’t? Have you had trouble sleeping or remembering things? That’s all it might take to catch it early.
Until then, the burden falls on patients and families to speak up. If you’re on steroids and your mood feels off - even a little - say something. Tell your pharmacist. Tell your nurse. Tell your doctor. It’s not ‘all in your head.’ It’s a biological reaction to a powerful drug. And it’s treatable - if you catch it in time.
Final Thought: This Isn’t Just About Pills
Corticosteroids save lives. They help people breathe, walk, and live with chronic disease. But like all powerful tools, they come with hidden costs. The real tragedy isn’t the psychosis itself - it’s that we don’t talk about it. We don’t screen for it. We don’t train doctors to look for it. And we don’t warn patients before they start.If you’re taking these meds, know the signs. If you’re caring for someone who is, watch for the subtle shifts - the sleeplessness, the sudden anger, the quiet withdrawal. These aren’t personality flaws. They’re warning signals. And they deserve attention - not dismissal.





Conor Forde
December 2, 2025 AT 23:51So let me get this straight - we’re giving people chemical fireworks to calm their asthma, then acting shocked when they start screaming at the toaster? I’ve seen a dude on prednisone try to negotiate with his cat like it was a UN delegate. This isn’t a side effect - it’s a feature they forgot to put in the manual. And no, your ‘stress’ isn’t making you hear voices. The pills are.
patrick sui
December 4, 2025 AT 18:38Interesting breakdown - the HPA axis disruption + dopamine surge mechanism is solid. But I’d argue we’re missing the epigenetic angle: chronic steroid exposure may alter GR (glucocorticoid receptor) methylation patterns in the hippocampus, leading to persistent dysregulation even after clearance. We’ve seen this in Cushing’s patients with lingering cognitive fog. Need more longitudinal neuroimaging studies.
Declan O Reilly
December 6, 2025 AT 08:37Man, I read this and thought of my uncle. Took 60mg of prednisone for his COPD flare. One day he was laughing at old sitcoms, next day he was convinced the FBI was bugging his dentures. He didn’t sleep for 72 hours. The doctor just said, ‘It’s the illness.’ Nah. It was the pills. He’s been fine since we tapered him down - but the damage? The fear? That’s still there. We need to stop treating this like a footnote.
James Steele
December 7, 2025 AT 07:35While the clinical phenomenology is well-documented, the epistemological framework underpinning this discourse remains woefully under-theorized. The conflation of pharmacological neurotoxicity with psychiatric nosology reflects a persistent biopsychosocial reductionism - a failure to acknowledge that steroid-induced psychosis is not a ‘disorder’ but an emergent property of endocrine disruption. We must decouple diagnosis from symptomatology and embrace a systems biology approach.
Shannon Gabrielle
December 8, 2025 AT 13:01Oh wow, a whole article about how drugs can make people crazy? Groundbreaking. Next you’ll tell us water can drown people. Maybe if you didn’t take 80mg of prednisone like it was candy, you wouldn’t turn into a paranoid lunatic. Stop blaming the medicine and start blaming the people who think they’re invincible.
ANN JACOBS
December 10, 2025 AT 02:52Thank you for this incredibly thorough and compassionate exploration of a critically under-discussed medical phenomenon. As someone who has watched a loved one navigate the terrifying labyrinth of steroid-induced psychiatric symptoms, I want to emphasize the profound importance of patient advocacy and early intervention. The fact that this is not routinely screened for speaks volumes about systemic gaps in healthcare - and I sincerely hope this article inspires policy change, educational reform, and greater empathy among clinicians.
Nnaemeka Kingsley
December 11, 2025 AT 16:09My cousin took steroid for swelling and started talking to walls. We thought he was drunk. Turned out it was the pills. He didn’t even know he was yelling at shadows. Doc said ‘wait and see.’ We waited 3 weeks. Bad call. He’s okay now, but we learned: if you feel weird on steroids, say something. No shame. It’s the drug, not you.
Sean McCarthy
December 12, 2025 AT 14:45Wait. So. You’re saying. That. Steroids. Can. Cause. Psychosis. In. People. Who. Don’t. Have. A. History. Of. Mental. Illness. And. This. Is. Not. Common. Knowledge. Among. Doctors. And. We. Are. Still. Prescribing. Them. Like. Candy. And. Not. Screening. For. This. At. All. And. No. One. Is. Doing. Anything. About. It.?
Jaswinder Singh
December 12, 2025 AT 20:29Bro this is real. My aunt got on steroids after a transplant and started crying for no reason then screamed at the TV like it was attacking her. We called the doc and they said ‘it’s normal’. Normal?! I’ve seen people go nuts on these pills and nobody’s talking about it like it’s a bomb. You think you’re just tired? Nah. You’re losing your mind. Tell someone. NOW.
Bee Floyd
December 14, 2025 AT 10:37I’ve been on low-dose prednisone for 18 months. Noticed the mood swings around month 6 - sudden rage, then euphoria, then numbness. Thought I was just burned out. Didn’t connect it until I read this. Tapered down slowly. Symptoms faded over 3 weeks. No psychosis, but the emotional rollercoaster? Real. I wish my rheumatologist had mentioned this. Just a heads-up could’ve saved me months of confusion.
Jeremy Butler
December 15, 2025 AT 04:16The ontological implications of exogenous glucocorticoid administration on the phenomenological structure of selfhood warrant serious philosophical inquiry. When the HPA axis is artificially coerced into suppression, the resultant neurochemical cascade not only alters affective states but fundamentally destabilizes the subject’s capacity for self-referential coherence. The psychotic episode, therefore, is not merely a symptom - it is an existential rupture induced by pharmacological hegemony.
Courtney Co
December 16, 2025 AT 10:45Wait so you’re saying I’m not just ‘dramatic’? That my panic attacks and hearing whispers when I’m on steroids isn’t just me being ‘too sensitive’? That it’s actually the drug? But… my doctor said I was just stressed. And I’ve been taking it for 3 years. So… am I crazy? Or is the system broken? I need someone to tell me I’m not imagining this. Please. I’m scared.