INR Target Range Calculator
Enter your INR value and select your condition to see if it's within your target range. This tool is based on standard medical guidelines for warfarin therapy.
Your INR Status
INR Value
Target Range
When you're on a blood thinner like warfarin, your life doesn't revolve around the medication itself - it revolves around a number: your INR. It’s not just a lab result. It’s the difference between staying safe and risking a stroke, or between avoiding a bleed and ending up in the hospital. This number tells your body whether it’s clotting too fast or too slow. And if you’re on warfarin, you need to know what that number means - and how to keep it right.
What Is INR, Really?
INR stands for International Normalized Ratio. It’s a standardized way to measure how long it takes your blood to clot. Before INR was invented in 1983, every lab used different chemicals to test blood clotting time. That meant your result in one hospital could be totally different from the same test at another. Patients got confused. Doctors made mistakes. The INR fixed that. Now, no matter where you get tested - whether it’s a big city hospital or a small clinic in rural New Zealand - an INR of 2.5 means the same thing everywhere.
The test starts with a simple blood draw or finger prick. The lab adds a substance that triggers clotting, then times how long it takes. That raw time is called the prothrombin time (PT). But PT alone doesn’t tell the full story. The INR formula adjusts that time using something called the ISI (International Sensitivity Index), which accounts for the specific reagent the lab uses. The result? A clean, universal number.
For someone not taking blood thinners, a normal INR is exactly 1.0. That’s your baseline. But if you’re on warfarin, your target is higher. Most people need to stay between 2.0 and 3.0. That’s the sweet spot: slow enough to prevent clots, fast enough to avoid bleeding. But not everyone’s target is the same.
Your Target INR Depends on Your Condition
One size doesn’t fit all. Your doctor picks your INR target based on what you’re being treated for.
- If you have atrial fibrillation (AFib), your target is usually 2.0-3.0.
- If you’ve had a deep vein thrombosis or pulmonary embolism, you’re also in the 2.0-3.0 range.
- If you have a mechanical mitral valve, your target jumps to 2.5-3.5 - tighter control is needed because these valves are more likely to cause clots.
- For a mechanical aortic valve, it’s still 2.0-3.0, but sometimes lower if you’re low-risk.
Why the difference? It’s about risk. Mechanical valves are made of metal and plastic - your body sees them as foreign. Clots form more easily on them. Atrial fibrillation increases clot risk too, but not as dramatically. That’s why the targets vary. Going too high increases bleeding risk. Too low, and you’re unprotected.
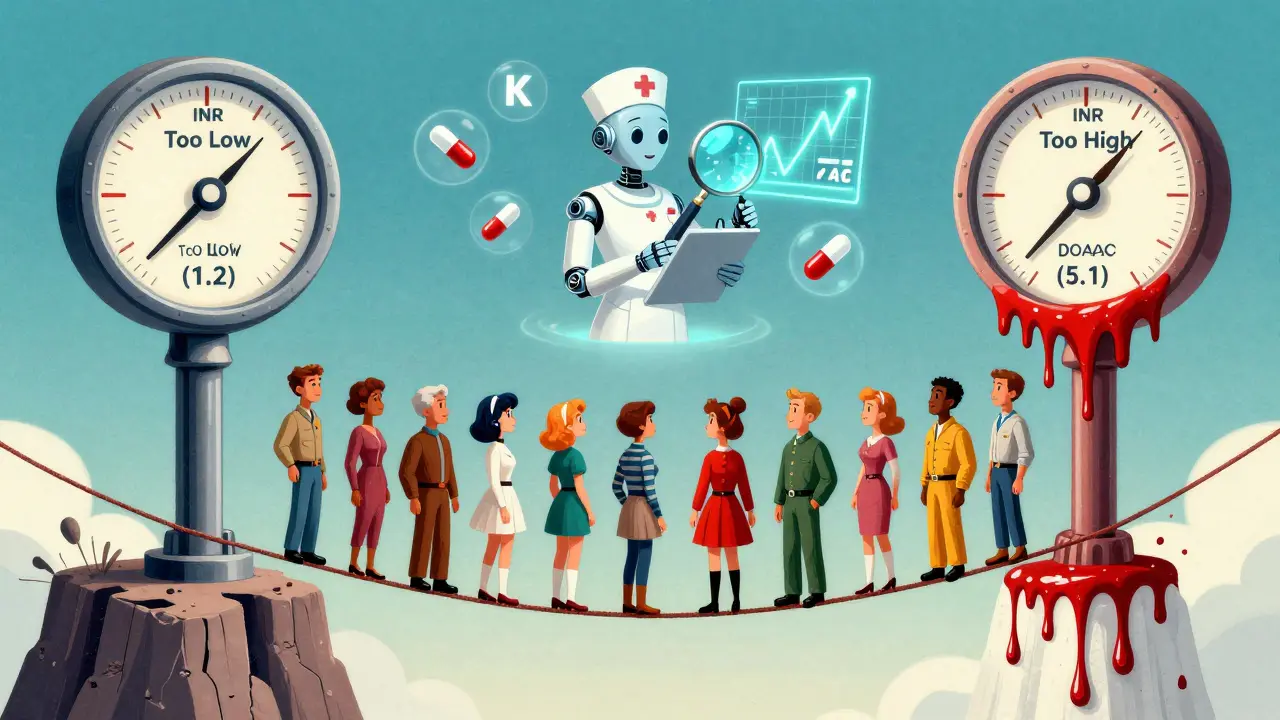
What Happens When Your INR Is Too High or Too Low?
Think of your INR like a tightrope. Step too far in either direction, and you fall.
If your INR is below 1.5, your blood is clotting too fast. You’re at risk for a stroke, heart attack, or a clot in your lungs or legs. This is rare on warfarin unless you’ve missed doses, started eating more vitamin K (found in leafy greens), or taken certain antibiotics that interfere with the drug.
If your INR is above 4.9, you’re in danger zone. Each 0.5-point rise above 3.0 increases your risk of major bleeding by 27%. That means nosebleeds that won’t stop, bruising without injury, blood in your urine or stool, or worse - bleeding in your brain. An INR over 5.0 is a medical alert. Your doctor will likely tell you to skip your next warfarin dose and get retested within 24 hours.
Studies show patients who stay within their target range 70% of the time cut their stroke risk by 42% and major bleeding by 28%. That’s not small. That’s life-changing.
Home Testing: Convenience vs. Complexity
For years, INR testing meant driving to a lab, waiting in line, and getting results days later. Now, home testing devices like the Roche CoaguChek and Abbott Acelis let you test yourself with a single drop of blood from your finger. The device gives a result in under a minute.
It sounds simple - and for many, it is. People who test at home spend 72% of their time in range, compared to 58% for those who rely on clinics. That means fewer clots, fewer bleeds, fewer hospital trips. One user on Reddit said, “I used to miss work every two weeks for a blood test. Now I do it while making coffee.”
But it’s not for everyone. If you have shaky hands, poor eyesight, or trouble remembering steps, home testing can backfire. The FDA found that 12% of home devices gave results more than 10% off from lab tests when INR was above 4.0 - exactly when you need the most accuracy.
Cost is another factor. The device costs around $300. Each test strip is $6. Medicare covers 100% if you qualify. Private insurance usually covers it too, but you might pay 20% coinsurance. Some people spend $1,500 a year out of pocket. For those on a fixed income, that adds up.
Warfarin vs. Newer Blood Thinners
There’s a quiet revolution happening in anticoagulation. Newer drugs - apixaban, rivaroxaban, dabigatran - don’t need INR monitoring. They’re called DOACs (Direct Oral Anticoagulants). They’re easier. No finger pricks. No weekly blood tests. Just take your pill and go.
But here’s the catch: DOACs aren’t right for everyone. If you have a mechanical heart valve, warfarin is still the only option. If your kidneys are failing, many DOACs are unsafe. And cost? Warfarin costs about $4 a month. DOACs? $550-$650. That’s a huge difference, especially without good insurance.
Also, DOACs have wider therapeutic windows. You don’t need to hit a narrow target like 2.5. You just take the dose, and it works. Warfarin? One missed dose, one extra serving of spinach, one new antibiotic - and your INR swings. That’s why it demands attention.
Still, DOACs are growing fast. In 2010, 70% of patients took warfarin. Today, it’s down to 30%. By 2028, 85% of new starts will be DOACs. But warfarin isn’t disappearing. It’s still essential for hundreds of thousands.

How to Stay in Range - Practical Tips
Keeping your INR stable isn’t magic. It’s routine.
- Test at the same time each day. Morning, after fasting 4-6 hours, is best. Your body’s clotting factors change throughout the day.
- Eat vitamin K consistently. Spinach, kale, broccoli - don’t avoid them. Just eat about the same amount every week. A sudden big bowl of salad can drop your INR. A sudden lack of greens can make it spike.
- Check every new medication. Antibiotics, painkillers, even herbal supplements like St. John’s Wort can interfere with warfarin. Always tell your pharmacist you’re on it.
- Track your INR. Write it down. Use an app. Know your trend. One high reading? Maybe a fluke. Three highs in a row? Call your doctor.
- Know your emergency numbers. If your INR is over 5.0, skip your next dose and call your provider immediately. Don’t wait.
And don’t over-test. A 2021 study found that 38% of stable warfarin patients get tested weekly - even though monthly is enough. Unnecessary testing doesn’t help. It just adds stress and cost.
The Bigger Picture: Access and Equity
Home INR testing is a game-changer - but only if you can get it. In urban areas, 82% of clinics offer full anticoagulation support. In rural areas? Just 35%. That gap isn’t just inconvenient. It’s dangerous. People without access are more likely to have out-of-range INRs. And that means more strokes, more bleeds, more deaths.
Technology is helping. The FDA approved a smartphone-connected INR monitor in early 2023 that sends results automatically to your doctor. AI tools are now predicting your next warfarin dose with 83% accuracy. But tech alone won’t fix inequality. Better access, better education, and better insurance coverage are needed.
Right now, 3.2 million Americans are on warfarin. About half are eligible for home testing. But only a fraction are using it. The same is true here in New Zealand. The tools exist. The evidence is clear. What’s missing is consistent support.
What’s Next?
If you’re on warfarin, your goal isn’t to get the perfect INR once. It’s to stay in range, day after day, month after month. That’s how you live longer, safer, and with fewer hospital visits.
Ask your doctor: Is home testing right for me? Can I get insurance coverage? Do I need training? Don’t assume you’re not a candidate. Many people who think they can’t do it - because of age, vision, or nerves - turn out to be great candidates with the right support.
And if your INR is stable? Celebrate. You’re doing something hard, every single day. You’re not just taking a pill. You’re managing a number that protects your life.
What is a normal INR level for someone not on blood thinners?
For someone not taking any anticoagulant medication, a normal INR is 1.0. This means their blood clots at the standard expected rate. Any value above 1.0 suggests the blood is taking longer to clot - which is intentional when someone is on warfarin.
Can I check my INR at home?
Yes, many people use FDA-approved home testing devices like the Roche CoaguChek or Abbott Acelis. These require a single drop of blood from a finger prick and give results in under a minute. Training is required, and not everyone is a good candidate - especially those with poor vision, shaky hands, or cognitive challenges.
Why does my INR change even when I take the same dose?
Warfarin is affected by many things: diet (especially vitamin K-rich foods like spinach), alcohol, other medications, illness, and even changes in your metabolism. A new antibiotic, skipping a meal, or drinking more than usual can all shift your INR. That’s why consistent habits matter more than perfect dosing.
What should I do if my INR is too high?
If your INR is above 5.0, skip your next warfarin dose and contact your healthcare provider immediately. Do not try to adjust the dose yourself. If you’re bleeding - nosebleed, bruising, blood in urine or stool - go to the emergency room. INR levels above 4.9 significantly increase bleeding risk.
Are there alternatives to warfarin that don’t require INR testing?
Yes, newer drugs called DOACs (like apixaban, rivaroxaban, and dabigatran) don’t require regular INR monitoring. They’re easier to manage but aren’t suitable for everyone - especially those with mechanical heart valves or severe kidney disease. Warfarin remains the only option for certain patients.
How often should I get my INR tested?
When you first start warfarin, you may need testing twice a week until your dose is stable. Once stable, most people test once a month. If you’re on home testing and your results are consistent, your doctor may extend it to every 6-8 weeks. Never test more often than needed - unnecessary testing adds stress without benefit.
Does insurance cover home INR testing?
Medicare Part B covers 100% of home INR testing for eligible patients with no deductible. Most private insurers also cover it, but you may pay 20% coinsurance. Coverage depends on your diagnosis, device type, and whether you’ve completed required training. Always check with your provider before buying a device.
Can I drink alcohol while on warfarin?
Moderate alcohol - one drink per day - is usually fine. But heavy or binge drinking can raise your INR and increase bleeding risk. Alcohol affects how your liver processes warfarin. If you drink regularly, tell your doctor. Sudden changes in alcohol intake can cause dangerous INR swings.





Phoebe McKenzie
January 2, 2026 AT 00:51Let me tell you something - if you’re not testing your INR at least twice a week, you’re playing Russian roulette with your brain. I’ve seen people die because they trusted their ‘stable’ numbers and skipped a test after eating kale. It’s not a suggestion, it’s survival. And don’t even get me started on those DOACs - big pharma pushed them because they make more money, not because they’re better. Warfarin is free, precise, and if you know what you’re doing, it’s the only real tool you need. Stop being lazy and test. Every. Single. Day.
gerard najera
January 3, 2026 AT 14:16INR isn’t a number. It’s a conversation between your liver, your diet, and your fate.
Stephen Gikuma
January 4, 2026 AT 18:26Ever wonder why the FDA lets these home devices exist? They’re not for you. They’re for the labs and the insurance companies. They want you testing at home so they can cut staff, cut costs, and dump the responsibility on the elderly. And don’t believe the ‘83% accuracy’ stat - that’s from a study funded by Roche. I’ve got a cousin who got a 5.8 reading at home and the clinic said 3.1. He almost bled out before they admitted the device was broken. They’re selling fear disguised as convenience.
Bobby Collins
January 5, 2026 AT 19:31ok but like… what if you just… don’t care? like i know my INR is always high but i just eat spinach and drink whiskey and it’s fine? my doctor says i’m a walking time bomb but i’m 72 and i’ve had 3 strokes already so… what’s the point? 🤷♀️
Layla Anna
January 6, 2026 AT 07:26my grandma did home testing for 8 years and never missed a day 😊 she’d take her coffee and prick her finger like it was yoga 🌿 she said the ritual kept her grounded. i used to think it was crazy but now i get it - it’s not about the number, it’s about showing up for yourself every day. love you grandma 💕
Heather Josey
January 7, 2026 AT 09:25This is one of the most comprehensive and clinically accurate overviews of warfarin management I’ve seen in a public forum. The distinction between mechanical valve targets and AFib is particularly well-articulated. For patients managing this long-term, consistency and documentation are not optional - they are foundational to survival. I encourage all providers to share this resource with their anticoagulation clinics. The equity discussion at the end is also critical - access should never be a privilege.
Lee M
January 8, 2026 AT 17:35You think you’re in control because you test every week? You’re not. You’re just a node in a system designed to keep you docile. The INR is a tool of surveillance - it tells the state you’re compliant, you’re obedient, you’re not a threat. The real danger isn’t clotting or bleeding - it’s surrendering your autonomy to a number that was invented by a committee in Geneva.
Kristen Russell
January 9, 2026 AT 16:28Home testing changed my life. I used to dread the lab. Now I do it before breakfast. I feel like I’ve got my power back. 🙌
Bryan Anderson
January 9, 2026 AT 22:28Thank you for this detailed breakdown. I’ve been on warfarin for 12 years and your explanation of the ISI and reagent variability clarified something my hematologist never fully explained. I’ve started using an INR tracking app and it’s helped me notice patterns - like how my levels dip every time I fly. Small insights, big impact.
Matthew Hekmatniaz
January 10, 2026 AT 15:23I’m from India and we don’t have easy access to home testing here. But I’ve seen people in rural villages manage warfarin with just a notebook, a calendar, and a community health worker who checks their INR once a month. It’s not perfect - but it’s human. Technology helps, but connection matters more. We don’t need fancy gadgets. We need people who care enough to show up.
Liam George
January 12, 2026 AT 05:05Let’s analyze the systemic architecture of anticoagulant governance. The INR paradigm is a hegemonic construct of the biomedical-industrial complex, leveraging the biopolitical control of coagulation kinetics to commodify patient compliance. The DOACs, while ostensibly eliminating monitoring, are merely shifting the burden of pharmacokinetic variance onto the patient’s metabolic resilience - a form of epistemic violence masked as convenience. The ISI, far from being a neutral index, is a calibrated instrument of pharmacological standardization designed to obscure regional variability in cytochrome P450 expression - a fact deliberately omitted from FDA labeling. The 70% in-range statistic? A statistical illusion constructed by cherry-picked cohorts in urban tertiary centers. The real crisis is not INR instability - it’s the erasure of patient epistemology in favor of algorithmic determinism.
Phoebe McKenzie
January 13, 2026 AT 04:14Of course Liam’s gonna write a 12-sentence manifesto. Meanwhile, people are dying because they trusted a $6 strip from a device that’s calibrated for someone in Minnesota, not their 80-year-old body in Arizona. You don’t need philosophy. You need a working meter and a doctor who doesn’t dismiss you. Stop overthinking. Start testing.