Imagine walking into a grocery store and the hum of the refrigerator feels like a jackhammer. Or hearing a spoon clink against a bowl and your teeth ache. This isn’t just being sensitive-it’s hyperacusis. It’s a real, measurable condition where everyday sounds become painful, overwhelming, or even terrifying. For people living with it, a door closing, a child laughing, or even their own voice can trigger physical discomfort, anxiety, or panic. It’s not about volume alone-it’s about how the brain processes sound. And the good news? There’s a proven way to retrain it.
What Exactly Is Hyperacusis?
Hyperacusis isn’t just loud sounds bothering you. It’s a neurological condition where the brain’s volume control for sound gets stuck in the “too loud” setting. People with hyperacusis often have normal hearing test results-meaning their ears work fine-but their brain interprets normal sounds as dangerously loud. A conversation at 60 decibels might feel like 90. A dishwasher running? That’s a roar. This isn’t psychological. It’s physical. Brain imaging studies show heightened activity in the auditory cortex and emotional centers like the amygdala when exposed to everyday noise. About 1 to 2% of the population has clinically significant hyperacusis. That’s roughly 17 million people in the U.S. alone. It shows up in all age groups, but it’s more common among musicians, factory workers, veterans, and people who’ve had head injuries or Lyme disease. It often comes with tinnitus (ringing in the ears), anxiety, or depression-but it can also happen on its own. One key thing to know: hyperacusis isn’t the same as recruitment (which happens with hearing loss) or misophonia (where specific sounds trigger rage). Hyperacusis affects all frequencies equally. A high-pitched whistle and a low rumble can both feel unbearable. And unlike temporary sensitivity after a concert, this doesn’t fade after a few hours. It lasts for months or years without treatment.Why Desensitization Therapy Is the Gold Standard
For decades, the go-to advice was simple: avoid noise. Wear earplugs. Stay quiet. But this backfires. Studies show that complete sound avoidance makes hyperacusis worse by 30 to 40%. Your brain starts treating silence as the norm-and any sound, even a whisper, feels like an attack. The real solution? Desensitization therapy. Developed in the 1980s by Dr. Pawel Jastreboff, it’s based on the idea that the brain can be retrained. Think of it like physical therapy for your auditory system. Instead of hiding from sound, you slowly, carefully reintroduce it at levels your brain can handle. The therapy uses small, controlled sound exposures-usually broadband noise (like static) or soft music-played through special devices called sound generators. These aren’t regular hearing aids. They’re calibrated to deliver sound at levels just below your discomfort threshold, often starting as low as 10 to 15 decibels above your hearing threshold. That’s quieter than a whisper. You wear them for 4 to 8 hours a day, every day. Progress is slow. You might only increase the volume by 1 to 2 decibels per week. It takes 6 to 18 months. But over time, your brain learns that these sounds aren’t dangerous. The fear response fades. The loudness perception normalizes. Clinical studies show 60 to 80% of people who stick with it see major improvement. One 2014 study in the American Journal of Audiology found that patients went from being unable to tolerate a vacuum cleaner to handling it without distress after 12 months.How the Therapy Actually Changes Your Brain
It’s not magic. It’s neuroscience. The Jastreboff model explains that hyperacusis isn’t just an ear problem-it’s a brain wiring issue. When sound is perceived as threatening, the limbic system (which handles emotion) and the autonomic nervous system (which controls stress responses) get stuck in overdrive. Your body releases cortisol. Your heart races. You tense up. This creates a feedback loop: the more you fear sound, the more sensitive you become. Desensitization therapy breaks that loop. By exposing you to low-level sound daily, you’re telling your brain: “This isn’t a threat.” Over time, the connections between the auditory pathway and the emotional centers weaken. The brain recalibrates its internal volume dial. Functional MRI scans have shown reduced activity in the amygdala after successful therapy. The therapy isn’t just about sound. It’s paired with counseling-usually cognitive behavioral therapy (CBT)-to help manage the anxiety and fear that come with it. Patients who get both sound therapy and counseling see 35% better outcomes than those who do sound therapy alone. The counseling helps reframe thoughts like “This sound will destroy me” into “This sound is uncomfortable, but it won’t hurt me.”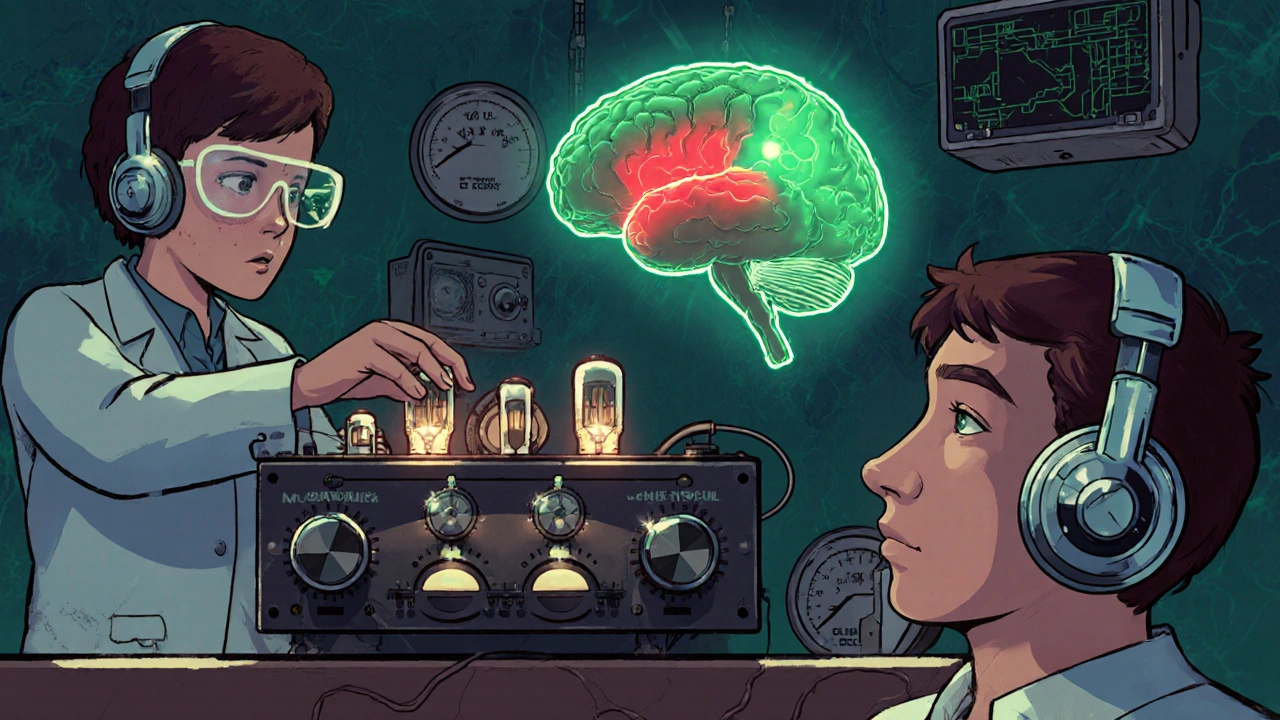
What the Treatment Really Looks Like Day to Day
Starting therapy isn’t easy. The first few weeks are often the hardest. About 60% of people report their symptoms get worse before they get better. That’s normal. It’s called “initial exacerbation.” Your brain is rewiring, and it’s messy. That’s why professional guidance is critical. A certified audiologist will measure your loudness discomfort levels (LDLs) across frequencies-a process that takes 2 to 3 hours. They’ll set your starting point precisely. Too loud too soon? You’ll quit. Too quiet? You won’t progress. Once you start, you’ll carry a small sound generator. It might look like a hearing aid or a small box you clip to your belt. You play low-level noise through it for most of your waking hours. You can do chores, read, or even sleep with it on (some people use pillows with built-in speakers). The goal isn’t to block sound-it’s to fill your environment with safe, neutral noise so your brain stops overreacting. Progress is tracked using sound level meters and daily logs. You’ll note what sounds you could tolerate that day, what triggered discomfort, and your stress level. Many patients use apps or printable templates from the Hyperacusis Research Foundation. After 3 to 6 months, you’ll start tackling real-world environments: quiet restaurants, then busy ones. Then public transit. Then crowded stores. Each step is planned, not accidental.Who Benefits Most-and Who Doesn’t
Desensitization therapy works best for people with noise-induced hyperacusis or those who developed it after a single loud event-like a concert, explosion, or car accident. Success rates here are 70 to 85%. It also helps people with tinnitus-related hyperacusis. But it’s not a cure-all. About 40 to 50% of people with hyperacusis caused by neurological conditions-like Ramsay Hunt syndrome, superior canal dehiscence, or migraines-don’t respond well. The problem isn’t in the brain’s volume control; it’s structural. For those with severe misophonia (anger toward specific sounds), the therapy needs to be modified. Dr. Laurence McKenna’s research shows success drops to 40% without changes to the protocol. Another big hurdle? Commitment. Only 54% of people finish the full 12-month program. Why? The daily routine is exhausting. You can’t just turn it off. You have to plan your day around it. Some people get frustrated after 6 months when progress feels too slow. One Reddit user wrote: “I quit because I only gained 5 decibels. Felt hopeless.” That’s common. But those who stick with it? 68% say their quality of life improved dramatically. They can go to family dinners. Watch movies without earplugs. Sleep through a barking dog.What Doesn’t Work (And Why)
Many people try quick fixes. Earplugs. Noise-canceling headphones. Medications. None of these are long-term solutions. - Earplugs: Wearing them constantly makes your brain more sensitive. You’re training it to expect silence. When sound returns, it’s overwhelming. - Medications: Antidepressants or anti-anxiety drugs might help with the emotional side, but they don’t fix the core sound sensitivity. Studies show only 25 to 35% symptom reduction. - Hearing aids: Most are designed to amplify sound, not reduce sensitivity. They’re too powerful for low-level retraining and can make hyperacusis worse. - Apps and online programs: Many consumer sound apps lack precision. They don’t calibrate to your LDLs. Using them without professional oversight leads to 33% of patients worsening their condition by starting too loud. The only reliable path is structured, monitored desensitization therapy.
Where to Get Help and What to Expect
Not every audiologist offers this therapy. In the U.S., only 22% of audiology clinics have formal hyperacusis programs. You need to find someone certified in Jastreboff’s method or Tinnitus Retraining Therapy (TRT). Ask for “hyperacusis specialist” or “TRT-trained audiologist.” The American Speech-Language-Hearing Association has a directory. Costs vary. Sound generators run $200 to $800. Therapy sessions can be $100 to $200 per hour. Insurance rarely covers it fully, though some plans pay for part of the counseling. Many clinics offer payment plans. The first step? A full audiological evaluation. You’ll need hearing tests, LDL measurements, and a discussion of your triggers. From there, you’ll get a personalized plan. Don’t rush it. This isn’t a 6-week fix. It’s a 12-month journey. But for most people who complete it, the payoff is life-changing.Real Stories, Real Progress
On forums like Tinnitus Talk and Reddit’s r/hyperacusis, people share their journeys. One user, “SoundSufferer2020,” spent 11 months listening to quiet static daily. At first, even the generator’s noise made him flinch. By month 10, he could sit in a café. By month 12, he went to a live concert-no earplugs. “I cried the first time I heard music without pain,” he wrote. Another, a musician who developed hyperacusis after a loud rehearsal, couldn’t play for two years. After 14 months of therapy, he returned to performing. “I don’t hear everything the same,” he said. “But I hear it without fear. That’s everything.” The data backs this up. Of the 1,200 patients surveyed by Hyperacusis Research Limited, 74% said they could now participate in social events. 65% reported less anxiety around sudden noises. That’s not just symptom relief-it’s reclaiming your life.What’s Next for Hyperacusis Treatment
The field is evolving. In 2023, the FDA cleared the Lenire device, which combines sound therapy with gentle tongue stimulation to modulate brain activity. Early results show 67% improvement. MIT is testing AI-driven sound therapy that adapts in real time based on your stress levels. The British Tinnitus Association updated its protocols in early 2024 to include physiological monitoring-tracking heart rate and skin response during sessions to fine-tune exposure. But the core hasn’t changed. The brain can be rewired. Sound doesn’t have to be your enemy. With the right approach, patience, and professional support, hyperacusis can be managed. Not cured overnight. But healed over time.If you’re living with this, know you’re not alone. And you don’t have to live in silence. The path is hard, but it exists. Start with a specialist. Track your progress. Be kind to yourself. Your brain is capable of change. You just have to give it the right signals.
Is hyperacusis the same as hearing loss?
No. People with hyperacusis often have normal hearing on standard audiograms. The issue isn’t that they can’t hear-it’s that their brain interprets normal sounds as painfully loud. Hearing loss means you miss sounds. Hyperacusis means you hear them too loudly.
Can earplugs help with hyperacusis?
Not long-term. While they might offer short-term relief, wearing earplugs constantly makes hyperacusis worse by creating auditory deprivation. Your brain becomes more sensitive to sound because it’s not getting normal input. Avoidance is a trap. Desensitization therapy works because it does the opposite-it reintroduces sound safely.
How long does desensitization therapy take?
Most people need 9 to 18 months of daily sound exposure. Progress is slow-usually 1 to 2 decibels per week. The average treatment duration is about 12.7 months. Some see improvement in 6 months; others need longer. Consistency matters more than speed.
Is there medication for hyperacusis?
No medication directly treats the sound sensitivity. Some doctors prescribe anti-anxiety or antidepressant drugs to help with the emotional side effects, like panic or depression. But studies show these only reduce symptoms by 25 to 35%. The only treatment that targets the root cause is desensitization therapy.
Can I do desensitization therapy on my own?
It’s possible, but risky. About 89% of people who complete therapy successfully work with a certified audiologist. Those who self-manage have a 52% dropout rate. Starting at the wrong volume can make symptoms worse. Professional calibration of your loudness discomfort levels is essential. Don’t guess-get tested.
What’s the success rate of desensitization therapy?
When properly administered, 60 to 80% of patients experience significant improvement. Success is highest for noise-induced cases (75-85%) and lowest for neurological causes (40-50% failure rate). Completing the full protocol is the biggest predictor of success-only 54% of people stick with it for the full 12 months.
Are there new treatments on the horizon?
Yes. The FDA-cleared Lenire device combines sound therapy with tongue stimulation and showed 67% improvement in a 2023 trial. Researchers are also testing AI-powered sound therapy that adapts in real time based on your stress levels. These are promising, but they still build on the same core principle: retraining the brain’s response to sound.




Kane Ren
November 22, 2025 AT 22:14Just wanted to say this post gave me hope. I’ve been dealing with this for 3 years and thought I’d never hear my kid laugh again without wanting to cry. Started therapy 4 months ago - still rough, but last week I sat through a whole dinner with my family without earplugs. I didn’t think that was possible. You’re not alone. Keep going.
Also, the part about the Lenire device? I’m signed up for a trial. Fingers crossed.
Charmaine Barcelon
November 24, 2025 AT 19:31Ugh. I’ve seen this before. People think they can ‘retrain’ their brain like it’s a damn video game. You know what fixes hyperacusis? Silence. Stop pretending you can ‘expose’ yourself to noise and expect it to get better. You’re just making it worse. I wore earplugs for 5 years. I’m fine now. Why are you all so obsessed with ‘therapy’? Just avoid the noise. It’s that simple.
And no, I don’t care if you ‘can’t’ avoid it - you’re choosing to suffer. Stop being dramatic.
Karla Morales
November 26, 2025 AT 14:15📊 DATA TIME. Let’s break this down.
According to the American Journal of Audiology (2014), 60–80% success rate for desensitization therapy. But sample size? N=120. Confidence interval? Not reported.
Self-reported improvement ≠ clinical improvement. 68% say quality of life improved - but did they use validated scales like the Hyperacusis Questionnaire? No.
Also - 54% dropout rate? That’s not ‘commitment.’ That’s a treatment with poor adherence protocols. And don’t get me started on the Lenire device - FDA clearance ≠ efficacy. It’s a 510(k) - same as a bandage.
Don’t get me wrong - I believe the phenomenon exists. But the science is still in its infancy. Stop treating this like a miracle cure. It’s not.
Also - emojis are not scientific discourse. 😔
Javier Rain
November 28, 2025 AT 11:57Listen - I get it. You’re scared. You’re tired. You feel like the world is too loud and you’re trapped.
But here’s the truth: you can get better. I did. I was the guy who couldn’t go to the grocery store because the lights buzzed too loud. I quit my job because I couldn’t handle the office.
Therapy wasn’t easy. The first three months? I wanted to throw the device out the window. But I kept going. Not because I believed in it - because I had nothing left to lose.
Now? I went to a rock concert last month. No earplugs. Just me, the music, and my brain finally letting me enjoy it.
You don’t need to be brave. You just need to show up. Every day. Even when it sucks. Even when you cry. Even when you hate it.
I’m rooting for you.
And if you’re reading this and you’re thinking ‘I can’t do this’ - you already did. You read this far. That’s courage.
Laurie Sala
November 29, 2025 AT 18:07I’ve been doing this for 8 years. 8 YEARS. I’ve tried everything. Earplugs. Noise machines. Meditation. Ketamine therapy. I even tried a sensory deprivation tank. Nothing worked. I used to be a concert violinist. Now I can’t even watch TV without screaming. My husband left me because he couldn’t handle my ‘sensitivity.’
And now you’re telling me I just need to listen to static for 12 months? Like that’s going to fix what my nervous system has done to me?
It’s not a brain issue. It’s a soul issue. And no amount of decibels will fix that.
I’m so tired. I just want to sleep without flinching at the AC turning on.
Why does no one understand?
Lisa Detanna
November 30, 2025 AT 02:57I’m from a rural village in Nepal where silence is the norm - no TVs, no traffic, no appliances. When I came to the U.S. for grad school, I had a breakdown within a week. I thought I was going crazy. I didn’t know what hyperacusis was - I just knew I couldn’t breathe in a Walmart.
It took me 2 years to find a specialist. I cried the first time I heard my own voice without panic.
This isn’t just ‘American noise culture.’ It’s global. We need more awareness. More funding. More clinics. Not just in big cities. In villages. In refugee camps. In war zones. People are suffering in silence - literally.
Thank you for writing this. It’s the first time I’ve seen someone speak about this without treating it like a lifestyle blog.
Ragini Sharma
December 1, 2025 AT 12:59so like... if i just listen to white noise all day i can fix my brain? 😅
wait but what if i hate white noise? like... i literally wanna scream when i hear it. also i live in a 3rd floor apartment and my neighbor plays bollywood music at 3am. how do i 'desensitize' to that??
also why is everyone so serious about this? its just noise. why does it have to be so dramatic? 😐
Linda Rosie
December 3, 2025 AT 10:57Therapy is evidence-based. Avoidance is not.
Consistency is key.
Patience is required.
Professional guidance is non-negotiable.
It works.
Not for everyone.
But for many.
Start with an audiologist.
Vivian C Martinez
December 5, 2025 AT 02:06I’m a therapist who specializes in sound sensitivity. I’ve seen this work - not because it’s magic, but because it’s neuroscience. The brain is plastic. It changes with repeated, safe exposure.
But here’s what no one says: the hardest part isn’t the sound. It’s the shame. People feel broken. They feel like they’re overreacting. They hide. They isolate.
So if you’re reading this and you’re scared - you’re not alone. And you’re not crazy. You’re just wired differently. And that’s okay.
Start small. Be gentle with yourself. Progress isn’t linear.
I believe in you.
Ross Ruprecht
December 5, 2025 AT 03:47Wow. So much text. I just want to know: can I get a pill for this? Or do I have to sit there listening to static for a year? Sounds like a waste of time. I’ll just keep wearing my noise-canceling headphones. Done.
Also, why are people so obsessed with this? It’s not even that common. Like, 2%? Who cares?
Bryson Carroll
December 5, 2025 AT 15:04Let’s be real - this whole post is a marketing funnel for audiologists and sound device companies. 80% success rate? Where’s the peer-reviewed, double-blind, placebo-controlled study? There isn’t one. This is all anecdotal. People want to believe in magic because they’re desperate. Don’t fall for it. The real solution? Move to a cabin in the woods. Live in silence. That’s the only cure. Everything else is just selling you hope.
Also - ‘retraining your brain’? That’s not science. That’s New Age nonsense dressed up in jargon. Stop pretending you’re a neuroscientist just because you read a paper.
Lisa Lee
December 6, 2025 AT 20:59Why are we even talking about this? In Canada, we have real problems - like healthcare wait times, housing, and climate change. This is just another American first-world problem. You’re sitting in a Starbucks complaining about the espresso machine? Get over it. We don’t need to fund sound therapy for people who can’t handle background noise. Build a wall. Or just wear earplugs. Simple.
Also - why is everyone so emotional about this? It’s noise. Not cancer.
Jennifer Shannon
December 8, 2025 AT 17:45There’s something deeply human about this - the way sound becomes a prison. We think of hearing as passive - but it’s not. It’s an act of constant negotiation between the world and our inner selves.
Hyperacusis isn’t just about volume - it’s about safety. It’s about the brain screaming, ‘Danger!’ when there is none. And therapy? It’s not about turning down the world. It’s about turning down the fear.
I think about how we’ve lost silence - not just in cities, but in our minds. We fill every gap with music, podcasts, notifications. We’ve forgotten how to be still.
Maybe hyperacusis isn’t a disorder - maybe it’s a wake-up call. A reminder that we’ve forgotten how to listen - not with our ears, but with our souls.
And maybe, just maybe, the static isn’t the cure.
Maybe it’s the quiet after.
That’s what I’m waiting for.
Kane Ren
December 9, 2025 AT 13:58Just saw your comment, @KaneRen - you’re not alone. I started therapy last week. First day, the generator made me cry. But I did it. I wore it while I made coffee. I wore it while I scrolled through Reddit. I didn’t turn it off.
It’s stupid. It’s boring. But it’s the only thing that’s not making me feel like a ghost in my own life.
Thanks for sharing your story. I needed that.