Hypercholesterolemia is a condition where your blood has abnormally high levels of cholesterol. This silent threat affects over 94 million Americans, yet nearly a third of them don't even know they have it. According to the World Health Organization, cardiovascular diseases linked to high cholesterol cause nearly 18 million deaths worldwide each year.
What is Hypercholesterolemia?
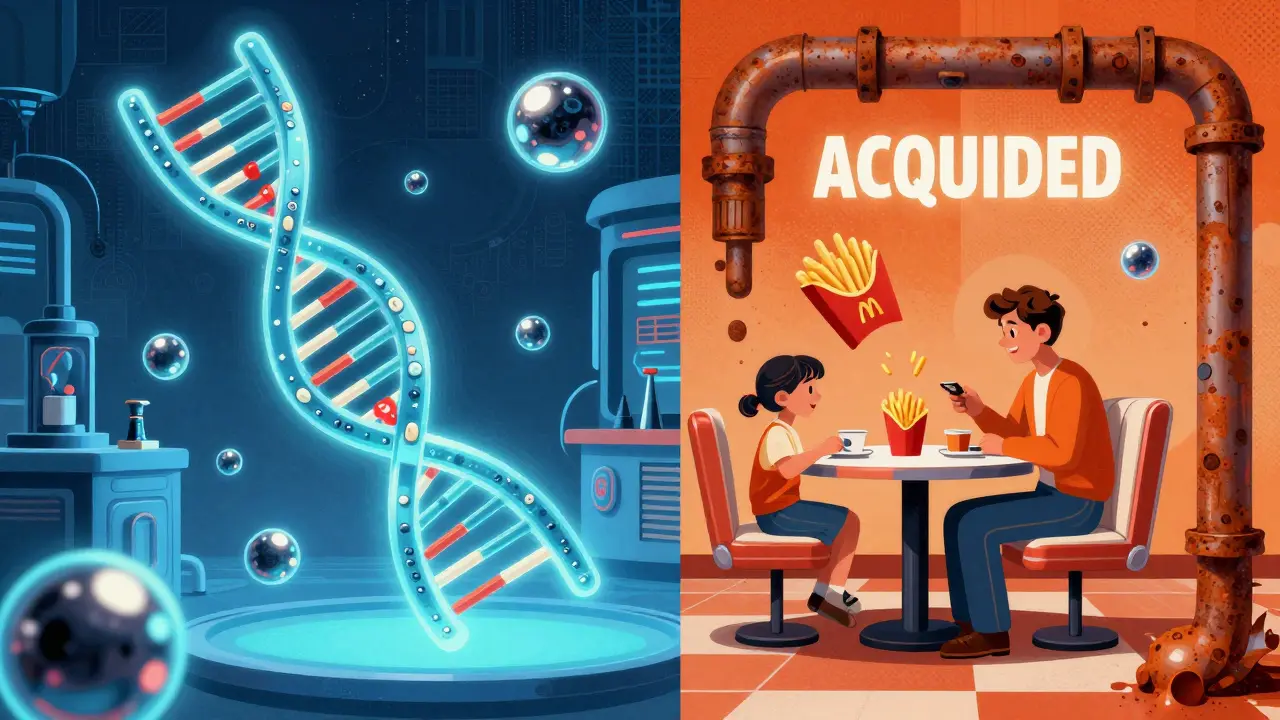
Hypercholesterolemia is defined as having total cholesterol levels above 200 mg/dL or LDL cholesterol above 100 mg/dL for most people. It's not a disease itself but a major risk factor for atherosclerotic cardiovascular disease. The American Heart Association reports that 93 million American adults aged 20 and older have total cholesterol exceeding 200 mg/dL. This condition has two main types: Familial Hypercholesterolemia (genetic) and acquired (lifestyle-related).
Why High Cholesterol is Dangerous
LDL cholesterol (low-density lipoprotein), often called "bad" cholesterol, builds up in your arteries. This creates plaque that narrows blood vessels, restricting blood flow to your heart and brain. Over time, this leads to heart attacks, strokes, or peripheral artery disease. The Global Burden of Disease Study 2019 found that atherosclerotic cardiovascular disease remains the top cause of death globally. Crucially, high cholesterol rarely causes symptoms until severe damage occurs-like when arteries are 70% blocked or more.
Types of Hypercholesterolemia
Not all high cholesterol is the same. Understanding the difference between genetic and acquired forms is key to effective treatment.
| Feature | Familial Hypercholesterolemia | Acquired Hypercholesterolemia |
|---|---|---|
| Primary Cause | Genetic mutations (LDLR, PCSK9 genes) | Lifestyle factors like poor diet, obesity, diabetes |
| Typical LDL Levels | 190-400 mg/dL (heterozygous), over 450 mg/dL (homozygous) | Usually below 190 mg/dL |
| Physical Signs | Tendon xanthomas (20-40% by age 30), xanthelasmas (50% of patients) | Usually no physical signs |
| Treatment Approach | Combination therapy: high-intensity statin, ezetimibe, PCSK9 inhibitors | Lifestyle changes first, then medication if needed |
Familial Hypercholesterolemia affects 1 in 250 people globally. It's caused by inherited gene mutations that prevent your body from removing LDL cholesterol properly. People with this condition often have extremely high LDL from birth. Untreated heterozygous FH increases heart disease risk 20-fold before age 40. Homozygous FH is rarer but far more severe-many patients experience heart attacks before age 20.
Acquired hypercholesterolemia stems from modifiable factors. Poor diet (especially saturated fats), lack of exercise, smoking, and conditions like diabetes or hypothyroidism raise LDL levels. For example, 68% of type 2 diabetics have dyslipidemia, and thiazide diuretics can increase LDL by 10-15%. Unlike genetic forms, lifestyle changes alone can often lower LDL by 10-15% for acquired cases.
How It's Diagnosed
A simple Lipid panel blood test measures total cholesterol, LDL, HDL ("good" cholesterol), and triglycerides. The U.S. Preventive Services Task Force recommends testing all adults aged 40-75 during cardiovascular risk assessments. Importantly, fasting isn't required for standard lipid panels anymore, making testing more accessible. For suspected familial hypercholesterolemia, genetic testing confirms mutations in LDLR or PCSK9 genes.
Lifestyle Changes That Work
Even with genetic forms, lifestyle changes support medication effectiveness. The Portfolio Diet-developed in JAMA Cardiology trials-lowers LDL by 10-15% through specific food combinations:
- 25 grams of soy protein daily (e.g., tofu, edamame)
- 10 grams of soluble fiber (oats, beans, psyllium)
- 2 grams of plant sterols (fortified foods)
- 15 grams of nuts (almonds, walnuts)
Regular exercise also helps. The American Heart Association recommends 150 minutes of moderate activity weekly, like brisk walking. This can lower LDL by 5-8% and boost HDL. Quitting smoking improves overall cardiovascular health within weeks. These changes are especially effective for acquired hypercholesterolemia.

Medication Options
When lifestyle changes aren't enough, medications become necessary. Statins are first-line treatment, reducing LDL by 30-60%. High-intensity options like atorvastatin (40-80 mg) or rosuvastatin (20-40 mg) achieve over 50% reduction, as shown in the IMPROVE-IT trial. For statin-intolerant patients (7-29% of users), alternatives include:
- Ezetimibe: Lowers LDL by 18% by blocking cholesterol absorption
- PCSK9 inhibitors (alirocumab, evolocumab): Injected monthly, they lower LDL by 50-60% and are often used for FH
Newer therapies like inclisiran (Leqvio) offer biannual injections, reducing LDL by 50% with better adherence. For severe FH cases, triple therapy (statin + ezetimibe + PCSK9 inhibitor) is standard. The Cleveland Clinic reports this approach helps 85% of FH patients reach target LDL levels.
Frequently Asked Questions
Can high cholesterol cause symptoms?
Typically, high cholesterol has no symptoms. It's called a silent killer because damage builds up in your arteries for years before you notice anything. By the time symptoms like chest pain or a heart attack occur, significant blockage has already developed. Physical signs like yellowish fatty deposits around the eyes (xanthelasmas) or on tendons (xanthomas) may appear in severe cases, especially with familial hypercholesterolemia.
How often should I check my cholesterol?
Adults aged 20+ should get tested every 4-6 years if risk is low. Those with risk factors (family history, diabetes, smoking) need testing every 1-2 years. After starting medication, check within 4-12 weeks to adjust doses, then every 3-12 months for ongoing management. The National Lipid Association confirms fasting isn't required for standard lipid panels, making testing easier.
What foods should I avoid to lower cholesterol?
Limit saturated fats (red meat, full-fat dairy) and trans fats (fried foods, baked goods). The Dietary Guidelines for Americans 2020-2025 removed the 300 mg/day cholesterol limit, but JAMA Internal Medicine studies show each 300 mg of dietary cholesterol per day increases heart disease risk by 17%. Focus on replacing these with unsaturated fats (avocados, olive oil) and fiber-rich foods like oats and beans.
Do statins have serious side effects?
Most people tolerate statins well. Muscle aches occur in 5-10% of users but are often mild. Severe side effects like liver damage or diabetes risk are extremely rare (less than 0.1%). A JAMA Internal Medicine review found statins save lives-every 39 mg/dL LDL reduction lowers major heart events by 22%. If side effects occur, switching to a different statin or adding ezetimibe usually resolves the issue.
Can children have high cholesterol?
Yes, especially with familial hypercholesterolemia. The American Academy of Pediatrics recommends screening children with family history of early heart disease or high cholesterol. Untreated FH in children leads to early atherosclerosis. Treatment includes diet changes and sometimes statins starting at age 8-10. Early intervention can prevent heart problems decades later.





Nancy Maneely
February 5, 2026 AT 12:16Ive been eating bacon for breakfast every day for 20 years. My cholesterol is high but I feel great. The WHO is just trying to push their agenda. In America we know better. Theyre all about selling drugs. I dont trust these stats. 94 million? That's made up. The real issue is the government controlling our food. But Im fine. Cholesterol isnt a big deal. Theyre just scaring people to sell statins. Ive got no symptoms so I dont care. The system is rigged.
Phoebe Norman
February 6, 2026 AT 08:17As a healthcare worker I've observed that statin side effects are underreported The data is manipulated Pharmaceutical companies control the narrative We need to address systemic issues Its a crisis People are dying Trust me I know Ive been in the field for years Its a scam
Albert Lua
February 7, 2026 AT 03:22Hey everyone! I'm from the Philippines and we eat a lot of fish and veggies. Our cholesterol levels are usually low. I think the US guidelines are too strict. It's all about the food we eat. We don't have heart disease problems like they do. The guidelines should be more culturally sensitive.
Katharine Meiler
February 7, 2026 AT 05:00Lipid management requires a nuanced approach. Elevated LDL is a marker but not sole determinant. Framingham risk score integrates factors. Statins for high-risk patients. Lifestyle modifications foundational. Evidence supports multi-modal strategy. Individualize treatment. Consider comorbidities. Holistic approach necessary.
Danielle Vila
February 7, 2026 AT 10:28The government is hiding the truth about cholesterol. It's all a scam to sell drugs. They're poisoning us with statins. I found a study that says cholesterol is good for you. The real cause of heart disease is sugar. They're covering it up. I read this article and it's all lies. The WHO is controlled by Big Pharma. They don't want us to know the truth. I've been researching this for years. It's a conspiracy. You're all being lied to.
Thorben Westerhuys
February 8, 2026 AT 21:22Oh my goodness!! This article is so important!!! I can't believe how many people are affected!!! It's terrifying!!! We need to act now!!! The statistics are alarming!!! 94 million Americans!!! That's almost one-third!!! It's a crisis!!! We must do something!!! Statins are life-saving!!! But also they have side effects!!! It's so complicated!!! I'm so worried!!! Everyone should get tested!!! Please!!! Please!!! Please!!!
Laissa Peixoto
February 10, 2026 AT 12:38It's interesting how we focus so much on cholesterol numbers. The real issue is systemic health. Cholesterol is just a symptom. We need to look at the bigger picture. Diet, exercise, stress management. The body is complex. Reducing it to numbers is reductive. Maybe we should focus on overall wellness. Just a thought. Not sure if it's helpful, but it's something to consider.
Samantha Beye
February 11, 2026 AT 22:05Hey, just wanted to say that managing cholesterol can be tough, but you're not alone. Small changes can make a big difference. Eating more veggies, walking regularly. It's all about progress, not perfection. You got this. Take it one step at a time. You're doing great.
Joyce cuypers
February 13, 2026 AT 05:49Hey, just wanted to say that managing cholestrol can be tough but your not alone. Small changes can make a big differnce. Eating more vegies, walking regularly. Its all about progress, not perfection. You got this. Take it one step at a time. Your doing great.
Tehya Wilson
February 13, 2026 AT 13:52The data is manipulated.
Johanna Pan
February 15, 2026 AT 05:24Hey everyone! In my culture we eat a lot of healthy foods like fruits and veggies. Cholesterol isnt the enemy. It's about balance. We should focus on whole foods. The US guidelines are too strict. But it's good that we're talking about this. Let's all make small changes. You can do it! It's not about perfection. Just take it step by step. I'm so optimistic about this. We can all improve our health together.