Aplastic anemia from medications is rare, but when it happens, it can turn deadly in weeks if ignored. It’s not just fatigue or a bad cold - it’s your bone marrow shutting down. No red blood cells to carry oxygen. No white blood cells to fight infection. No platelets to stop bleeding. And the trigger? A drug you took for something else - maybe antibiotics, seizure meds, or even common painkillers. The worst part? Most people don’t realize what’s happening until it’s too late.
What Exactly Is Medication-Induced Aplastic Anemia?
Aplastic anemia means your bone marrow - the soft tissue inside your bones - stops making blood cells. Not just a little. Not temporarily. Completely. Medications can cause this by either poisoning the stem cells directly or tricking your immune system into attacking them. It’s not the same as chemo side effects, which usually bounce back. This is different. Once it starts, it doesn’t fix itself without intervention.
Chloramphenicol, an old antibiotic, was the first drug linked to this in the 1950s. Today, carbamazepine (used for epilepsy), sulfonamide antibiotics, gold salts (for rheumatoid arthritis), and even some NSAIDs like ibuprofen in rare cases can trigger it. The risk is low - about 1 in 24,000 for chloramphenicol, 1 in 10,000 for carbamazepine - but when it hits, it hits hard. About 70% of these cases are classified as severe, meaning your blood counts drop below life-threatening levels.
Early Signs You Can’t Afford to Ignore
People often brush off the first signs. “I’m just tired.” “I’ve been stressed.” “I caught a bug.” But here’s what’s different with medication-induced aplastic anemia: the symptoms don’t go away. They get worse, slowly at first, then fast.
- Unrelenting fatigue - You sleep 10 hours and still feel drained. Walking to the mailbox leaves you breathless.
- Easy bruising - You didn’t bump into anything, yet your legs are covered in purple spots. Tiny red dots (petechiae) appear on your ankles.
- Recurrent fevers - Low-grade fevers (99-101°F) that come and go, no cough, no sore throat. Your body is fighting invisible infections.
- Bleeding gums or nosebleeds - Minor brushing triggers bleeding. Nosebleeds last longer than 10 minutes.
- Unexplained weight loss - Losing 5-10 pounds over 2-3 weeks without trying.
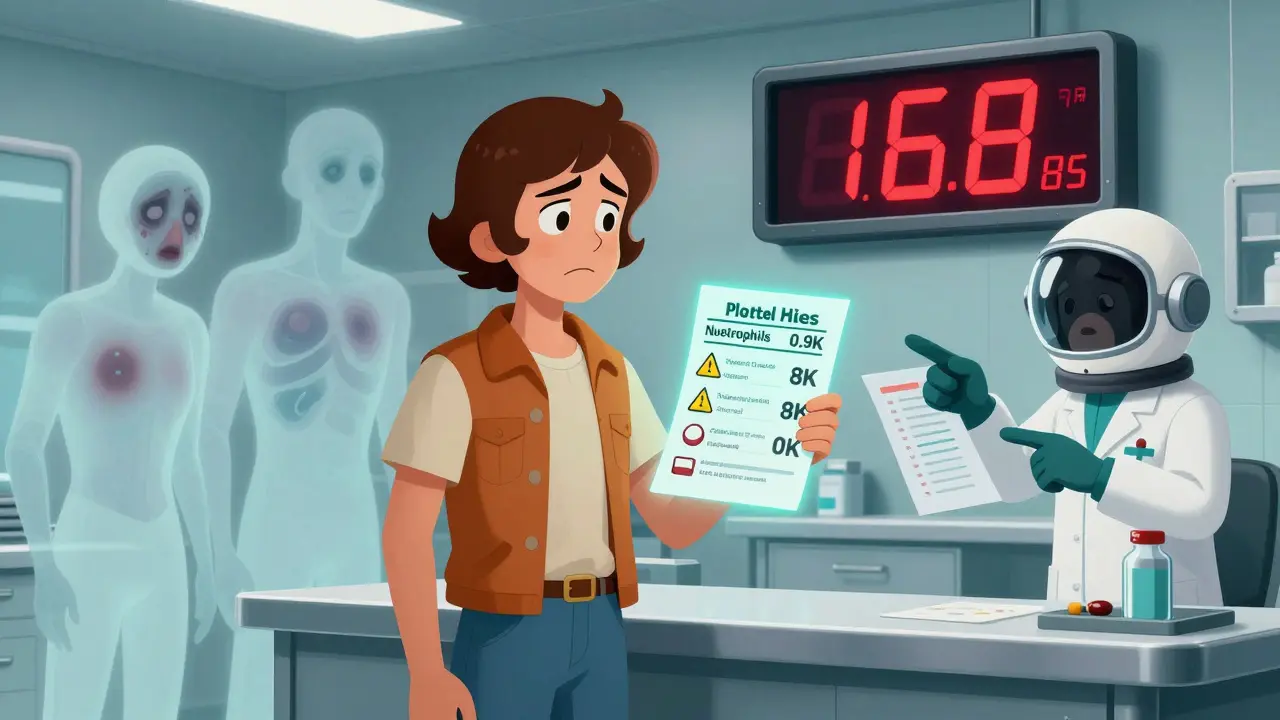
These aren’t random. They’re your body screaming. The bone marrow is failing. Blood counts are dropping. And the scary part? Lab changes happen before you feel sick. A CBC test might show low platelets or neutrophils weeks before you notice symptoms.
Which Medications Are Most Likely to Cause This?
Not every drug causes this. But some carry well-documented risks. Here are the top offenders:
- Chloramphenicol - Highest risk. Even short courses can trigger it. Rarely used now, but still found in some topical ointments.
- Carbamazepine and phenytoin - Common seizure meds. Immune system gets confused and attacks stem cells.
- Sulfonamide antibiotics - Like Bactrim or Septra. Used for UTIs, sinus infections.
- Gold compounds - Used for rheumatoid arthritis. Often forgotten as a risk.
- NSAIDs - Ibuprofen, naproxen. Risk is low, but documented in case reports.
- Some antipsychotics - Like clozapine. Requires regular blood monitoring for this reason.
Chemotherapy drugs cause bone marrow suppression - that’s expected. But aplastic anemia is different. It’s not just suppression. It’s permanent failure to recover, even after stopping the drug. That’s the line.
What to Do Immediately If You Suspect It
If you’re on any of these meds and you have two or more of the symptoms above, don’t wait. Don’t call your doctor tomorrow. Act now.
- Stop the medication. Immediately. Don’t wait for approval. This is the single most important step. Studies show 85% of mild cases start recovering within 4 weeks of stopping the drug.
- Get a CBC test within 24 hours. This isn’t optional. Ask for a complete blood count - hemoglobin, platelets, neutrophils. If your neutrophils are below 1,500/μL or platelets below 150,000/μL, you need a hematologist today.
- Go to the ER if you have a fever over 100.4°F. In aplastic anemia, even a low fever can mean a deadly infection. Your immune system can’t fight back. This is a medical emergency. Don’t drive yourself. Call an ambulance.
- Bring your medication list. Write down every pill, supplement, and topical cream you’ve taken in the last 3 months. Pharmacists and ER staff need this. One patient’s diagnosis was made because her pharmacist noticed she’d been on Bactrim for 6 weeks and asked about bruising.
Don’t rely on your primary care doctor to catch this. Only 47% of family doctors can name the top five drugs linked to aplastic anemia. You have to be your own advocate.
What Happens After Diagnosis?
If your CBC shows pancytopenia (low in all three blood types), you’ll be referred to a hematologist. They’ll order a bone marrow biopsy - the only way to confirm aplastic anemia. The marrow should be empty, less than 25% cellularity. If it is, you’re diagnosed.
Treatment depends on severity:
- Mild cases: Stop the drug, monitor blood counts weekly. Recovery often happens in 6-12 weeks.
- Severe cases: Immunosuppressive therapy - horse anti-thymocyte globulin (ATG) plus cyclosporine. This stops your immune system from destroying your marrow. Response rates are now 78% with this combo.
- Very severe cases: Bone marrow transplant. Especially if you’re under 40 and have a matched sibling donor. Survival rates hit 90% with early transplant.
And here’s the hard truth: restarting the drug that caused it? 90% chance of a worse relapse. Never do it. Ever.

Why Most People Are Diagnosed Too Late
It’s not because doctors are careless. It’s because the symptoms look like everything else. In one survey, 68% of patients had their symptoms dismissed as stress, viral illness, or depression. Pediatric cases are even worse - parents think it’s just growing pains or a lingering cold.
Patients who waited more than 3 weeks to get tested had a 62% survival rate. Those who got tested within a week? 89%. Time isn’t just a factor - it’s the difference between life and death.
One patient, 52, took ibuprofen daily for back pain. She started feeling tired, got a few bruises, ignored it. Three weeks later, she collapsed from internal bleeding. Her platelets were at 8,000. She needed a transplant. She’s alive now - but she almost didn’t make it.
How to Protect Yourself
If you’re starting a high-risk medication - carbamazepine, sulfonamides, gold therapy - ask for a baseline CBC before you begin. Then, get tested again after 2 weeks and again at 4 weeks. That’s the window when damage shows up.
Keep a medication log. Use a phone app if you need to. The AAMDS Foundation has a free one that tracks symptoms and blood counts. Users reduced diagnostic delays by 40%.
Know your family history. Aplastic anemia can run in families - but medication-induced cases are usually isolated. Still, if you’ve had low blood counts before, be extra cautious.
And if you’re ever unsure? Call a hematologist. Don’t wait for your GP to refer you. Call directly. Most clinics will see you within 24 hours if you say, “I’m on [drug] and I have low blood counts.”
Final Reality Check
Medication-induced aplastic anemia is preventable. It’s not a mystery. It’s not inevitable. It’s a warning sign you can act on - if you know what to look for.
Most people who survive it didn’t get lucky. They acted fast. They asked the right questions. They refused to let fatigue slide.
If you’re on one of these drugs and you feel off - really off - don’t wait. Don’t hope it passes. Get a blood test. Today.
Can over-the-counter painkillers like ibuprofen cause aplastic anemia?
Yes, though it’s rare. NSAIDs like ibuprofen and naproxen have been linked to cases of aplastic anemia in medical literature. The risk is extremely low - far lower than with drugs like carbamazepine or chloramphenicol - but it’s documented. If you’ve been taking high doses for months and notice unexplained bruising, fatigue, or fevers, stop the medication and get a CBC test immediately.
How long after stopping the drug does recovery begin?
In mild cases, blood counts often start improving within 2-4 weeks after stopping the medication. Full recovery can take 3-6 months. In severe cases, recovery depends on treatment like immunosuppressive therapy or transplant. Waiting longer than 4 weeks without intervention increases the risk of progression to life-threatening levels.
Is aplastic anemia from medication permanent?
Not always. About 60-70% of patients recover fully after stopping the drug and receiving treatment. Recovery depends on early detection, severity at diagnosis, and how quickly treatment starts. Some patients need long-term medication like cyclosporine, and a small percentage require bone marrow transplants. But with prompt action, long-term survival exceeds 85%.
Can you get aplastic anemia from antibiotics like amoxicillin?
Amoxicillin is not commonly linked to aplastic anemia. The antibiotics with the strongest evidence are sulfonamides (like Bactrim) and chloramphenicol. Amoxicillin can cause mild, temporary drops in white blood cells - but not the persistent, multi-lineage failure seen in true aplastic anemia. Still, if you develop unexplained bruising or fever while on any antibiotic, get checked.
Should I avoid all medications that have been linked to aplastic anemia?
No. These drugs are still used because they work - and the risk is very low for most people. The key is awareness. If you’re prescribed one of these medications, ask your doctor if you need baseline or follow-up blood tests. Know the warning signs. Don’t panic - but don’t ignore symptoms either. For many, these drugs are lifesaving. The goal isn’t to avoid them, but to use them safely.
What’s the survival rate if it’s caught early?
If diagnosed and treated within 2 weeks of symptom onset, survival rates are below 10%. If diagnosis is delayed beyond 8 weeks, mortality jumps to 45%. Early detection - through blood tests and quick action - is the single biggest factor in survival. With modern treatments, 5-year survival for medication-induced cases now exceeds 85%.





Winni Victor
December 24, 2025 AT 18:07So let me get this straight - ibuprofen is now on the same level as chloramphenicol? My grandma took two Advil a day for 40 years and still beat cancer at 89. You’re scaring people into ditching OTC meds like they’re radioactive. I’ve got bruises from hugging my cat. So what? I’m not dying. I’m just… bruised. And also mildly annoyed by fearmongering dressed as medical advice.
Linda B.
December 25, 2025 AT 17:21They don’t want you to know this but the FDA quietly banned chloramphenicol in 1982 because Big Pharma knew it was too effective - and too cheap. Now they’ve replaced it with carbamazepine and NSAIDs because they make more money off chronic treatment. The real cause? Glyphosate in your water. It’s not the drug - it’s the toxin buildup. You think your CBC is low because of ibuprofen? It’s because your liver is coated in pesticide sludge. Ask your doctor if they’ve ever tested for heavy metals. They haven’t. Because they’re paid by the labs.
Christopher King
December 27, 2025 AT 11:47Let’s be real - this isn’t about medicine. This is about control. They want you dependent. They want you scared. They want you coming back every month for another blood test, another prescription, another $300 copay. Aplastic anemia? It’s not the drug. It’s the system. The bone marrow doesn’t shut down because of Bactrim - it shuts down because your soul is tired of being told what to take. You think you’re fighting a disease? You’re fighting a machine. And the only cure? Walk away. From the pills. From the doctors. From the fear. Find a forest. Breathe. Let your body remember how to heal itself.
Michael Dillon
December 27, 2025 AT 15:52I’ve been on naproxen for three years for my back. Never had a single bruise. Never had a fever. Never even felt weird. I’m not saying it’s impossible - I’m saying it’s statistically absurd to panic over one in 24,000. If you’re gonna stress about meds, start with the ones you’re actually on for depression. Those have a 1 in 500 chance of killing you. This? This is just fear porn. You want to save lives? Stop posting this on Reddit. Go to a clinic. Volunteer. Do something real.
Gary Hartung
December 28, 2025 AT 23:45It is, of course, profoundly unfortunate - nay, tragic - that the modern medical-industrial complex has so thoroughly commodified human suffering that even the most benign pharmaceuticals are now subject to apocalyptic narratives propagated by anonymous internet users with access to PubMed and a flair for melodrama. One must ask: who benefits? The pharmaceutical corporations? The hematologists? Or the algorithm that thrives on dread? The answer, as always, is the same: the attention economy. And we, the unwitting subjects, are its most compliant currency.
Ben Harris
December 30, 2025 AT 10:26I was on Bactrim for a UTI and started bleeding from my gums. I didn’t think twice. Went to the ER. Platelets at 12K. They said I was lucky. Lucky? I was almost dead. I didn’t know this stuff. No one told me. My doctor just said ‘take the pill.’ I’m alive now because I Googled ‘bruising + fever + antibiotics’ at 3AM. That’s not medical care. That’s survival by accident. If you’re on these meds, check your blood. Now. Don’t wait until you’re on a gurney.
Carlos Narvaez
December 30, 2025 AT 14:59Carbamazepine risk: 1 in 10,000. Ibuprofen: 1 in 1,000,000. The math doesn’t support the panic. Awareness is good. Fear is not. If you’re on a high-risk drug, get baseline labs. That’s it. Don’t turn every bruise into a death sentence. Most people who take NSAIDs live to 80. And they didn’t need a hematologist to do it.
Zabihullah Saleh
January 1, 2026 AT 06:33In my village in Afghanistan, we used to say: ‘The medicine that heals can also bury you.’ We didn’t have labs or CT scans. We had elders. We had patience. We watched. We waited. We didn’t panic at every bruise. We didn’t call 911 for a fever. We gave tea, rest, time. Maybe we lost some. But we didn’t lose our peace. Today, we have more tests but less wisdom. Maybe the real illness isn’t in the marrow - it’s in the hurry.
Sophie Stallkind
January 2, 2026 AT 14:23Thank you for this comprehensive and clinically accurate overview. The distinction between drug-induced bone marrow suppression and true aplastic anemia is often misunderstood even among healthcare professionals. I would respectfully suggest that patients on high-risk medications be provided with a printed patient information sheet at the time of prescription, outlining the warning signs and immediate actions to take. This could significantly reduce diagnostic delays and improve outcomes. The AAMDS Foundation’s tracking tool is an excellent resource and should be promoted more widely by primary care networks.
Katherine Blumhardt
January 3, 2026 AT 02:06ok so i took ibuprofen for a week and now i have a tiny red dot on my ankle?? am i dying?? like?? i think im gonna cry?? i just wanted to stop my headache?? why is everyone so dramatic?? also i think the moon is made of cheese and i’m allergic to wifi
sagar patel
January 3, 2026 AT 18:57Low platelets from NSAIDs are documented in case reports. But the risk is negligible. The real issue is overdiagnosis. People panic over minor CBC abnormalities. I’ve seen patients referred to hematologists because their hemoglobin was 13.2. They’re not anemic. They’re just normal. This post amplifies anxiety. Not awareness.
Bailey Adkison
January 4, 2026 AT 04:39You say don’t wait. But you also say stop the drug immediately. What if you’re on it for seizures? What if stopping causes a seizure? You’re giving medical advice without context. That’s dangerous. You don’t get to play god because you read a study. If you’re on carbamazepine and feel off - talk to your neurologist. Not Reddit. Not your cousin who googled ‘bone marrow failure.’
Oluwatosin Ayodele
January 4, 2026 AT 23:52In Nigeria, we don’t have access to CBC tests every two weeks. We don’t have hematologists in every town. We have mothers who pray when their children get tired. We have men who swallow antibiotics because they have no choice. Your ‘urgent actions’ are a luxury. This post is beautiful. But it’s for the rich. The rest of us? We survive anyway. Don’t preach to us like we’re careless. We’re just poor.
Jason Jasper
January 5, 2026 AT 01:18I’ve been on clozapine for 12 years. I get my blood drawn every week. I know the numbers. I know the risks. I’m alive because I didn’t ignore them. I didn’t panic. I didn’t stop cold turkey. I worked with my team. This post is helpful. But it’s not about fear. It’s about partnership. Between patient and doctor. Between awareness and action. Don’t just stop the drug. Talk to someone who knows your history. That’s the real lifeline.