Every fall, millions of people reach for antihistamines to fight sneezing, itchy eyes, and runny noses. But not all antihistamines are the same. Some knock you out. Others let you drive, work, or pick up your kids without a second thought. Knowing which one to pick - and how to use it safely - can make all the difference.
What Are Antihistamines and How Do They Work?
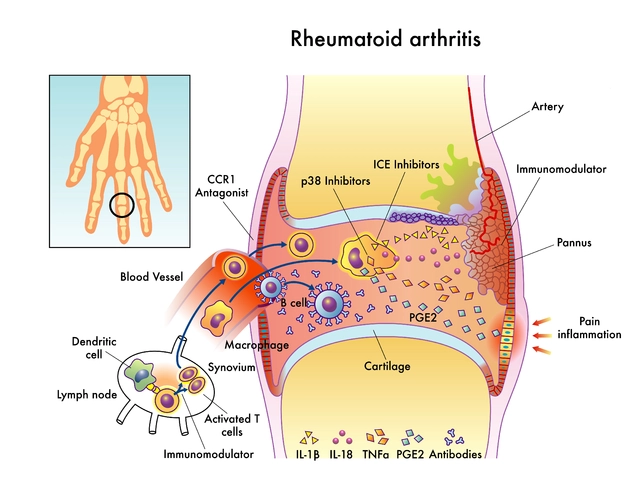
Antihistamines block histamine, a chemical your body releases during an allergic reaction. When pollen, dust, or pet dander triggers your immune system, histamine rushes out and causes swelling, itching, and mucus production. Antihistamines stop histamine from binding to receptors, calming those symptoms before they get out of hand.
There are two main types: H1 and H2. H1 antihistamines are what you find on pharmacy shelves for allergies. H2 antihistamines, like famotidine (Pepcid), target stomach acid and are used for heartburn. This guide focuses on H1 antihistamines - the ones you take for hay fever, hives, or seasonal allergies.
First-Generation vs. Second- and Third-Generation Antihistamines
The big divide in antihistamines comes down to whether they cross into your brain. First-generation antihistamines like diphenhydramine (Benadryl), chlorpheniramine (Chlor-Trimeton), and doxylamine (Unisom) are designed to enter the brain. That’s why they cause drowsiness - and why they’re also used as sleep aids.
Second- and third-generation antihistamines - like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) - were developed to avoid the brain. They’re less likely to make you sleepy because they can’t easily cross the blood-brain barrier. Studies show that diphenhydramine has nearly three times the brain penetration of fexofenadine. That’s why one makes you nod off, and the other lets you stay sharp.
Here’s the catch: even among the non-sedating options, some still cause drowsiness in certain people. Cetirizine (Zyrtec), for example, causes drowsiness in about 14% of users, while fexofenadine (Allegra) only affects 6%. That’s why some people swear by Allegra - they get relief without the fog.
Which Antihistamine Works Best?
There’s no single “best” antihistamine - it depends on your body and your lifestyle.
- Fexofenadine (Allegra): Lowest risk of drowsiness. Ideal for truck drivers, surgeons, or anyone who can’t afford to feel sluggish. Works in 1-2 hours and lasts 24 hours. Also the only OTC antihistamine officially labeled for hives, though all work for that.
- Loratadine (Claritin): Reliable, affordable, and widely available. Starts working in about an hour. Minimal sedation risk. A top pick for daily use.
- Cetirizine (Zyrtec): Fast-acting and potent. But it’s the most likely to cause drowsiness among the non-sedating group. Many users report feeling tired by mid-afternoon.
- Levocetirizine (Xyzal): A stronger version of Zyrtec. Works faster and lasts longer, but comes with stronger warnings for older adults. Not recommended for people over 65 without a doctor’s advice.
- Diphenhydramine (Benadryl): Works fast - within 15-30 minutes. Great for sudden reactions. But it’s not for daily use. Studies show it impairs driving as much as a 0.10% blood alcohol level. Avoid if you need to be alert.
Real users back this up. On Reddit’s r/Allergies, 78% of positive Allegra reviews mention zero drowsiness. Meanwhile, 65% of negative Zyrtec reviews say it made them sleepy. Amazon ratings show Claritin with a 4.4/5 average from over 28,000 reviews, while Benadryl sits at 3.9/5 with complaints about being “knocked out completely.”
When and How to Take Them
Timing matters more than you think. If you wait until your nose is running and your eyes are watering, you’re already behind.
Experts recommend starting your antihistamine 1-2 weeks before pollen season begins. This stops histamine receptors from getting overwhelmed. Think of it like putting on sunscreen before going to the beach - you’re preventing damage, not just treating it.
Dosing is simple for most OTC options: one tablet per day. But first-generation antihistamines often require dosing every 4-6 hours. That’s not practical for daily life - and it increases your risk of side effects.
Also, avoid grapefruit juice with antihistamines like fexofenadine. It can raise blood levels by up to 37%, increasing side effect risks. Stick with water.
Who Should Avoid Antihistamines?
Not everyone can safely use OTC antihistamines.
- Children under 6: First-generation antihistamines are not safe for young kids. The American Academy of Pediatrics warns they can cause seizures, rapid heart rate, or even death in toddlers.
- Adults over 65: Older adults are more sensitive to drowsiness. Xyzal’s OTC label doesn’t even include dosing instructions for this group. Even Zyrtec can cause confusion or falls in seniors.
- People with glaucoma, enlarged prostate, or thyroid issues: Antihistamines can worsen these conditions. Talk to your doctor before starting.
- Pregnant or breastfeeding women: While some antihistamines are considered low-risk, always check with your provider. Loratadine and cetirizine are often preferred, but individual advice matters.
Side Effects and Risks
Non-sedating antihistamines are generally safe, but they’re not risk-free.
Common side effects include dry mouth, headache, and mild stomach upset. These are usually minor and go away with time.
More serious risks? Drowsiness. Even “non-sedating” options like Zyrtec can make you tired. That’s why the FDA requires all OTC antihistamine labels to say: “Do not operate heavy machinery if drowsiness occurs.”
Long-term use? No major red flags yet. But some studies suggest chronic use of first-generation antihistamines might be linked to a slightly higher dementia risk in people over 75. The evidence isn’t conclusive - and it doesn’t apply to second-generation drugs. Still, if you’re taking Benadryl every night for years, it’s worth discussing with your doctor.

When to See a Doctor
OTC antihistamines are great for mild to moderate allergies. But if you’re still struggling after 2-3 weeks, or if you need them year-round, it’s time to talk to an allergist.
Also, see a doctor if you experience:
- Difficulty breathing or swelling of the face, lips, or throat
- Heart palpitations or chest pain
- Severe dizziness or confusion
- Symptoms that don’t improve with OTC meds
For chronic hives or severe seasonal allergies, biologic drugs like Xolair or Dupixent may be options - but those require prescriptions and specialist care.
Smart Tips for Safe Use
- Start with a non-sedating option like Claritin or Allegra before trying anything stronger.
- Don’t mix antihistamines with alcohol - it multiplies drowsiness.
- Check labels for hidden antihistamines in cold and flu medicines. Taking two products with diphenhydramine can lead to overdose.
- Use apps like the AAAAI’s “Allergy Relief Finder” to compare options based on your symptoms and job.
- Keep a journal: note which antihistamine you took, when, and how you felt. It helps you and your doctor find the right fit.
Most people find relief within a few days. If one doesn’t work, try another. About 30% of users need to test two or three before finding the one that fits their body.
Can I take antihistamines every day?
Yes, second- and third-generation antihistamines like Claritin, Zyrtec, and Allegra are safe for daily use. They’re designed for long-term allergy management. First-generation options like Benadryl are not recommended for daily use due to drowsiness and cognitive side effects.
Which antihistamine is least likely to make me sleepy?
Fexofenadine (Allegra) has the lowest risk of drowsiness among OTC antihistamines. Clinical studies show only 6% of users report feeling sleepy, compared to 14% for cetirizine (Zyrtec) and up to 18% for first-generation options.
Is Zyrtec better than Claritin?
Zyrtec (cetirizine) works faster and may be slightly more effective for some people, but it causes drowsiness more often than Claritin (loratadine). Claritin is the safer daily choice if you need to stay alert. Neither is universally better - it depends on your tolerance for side effects.
Can children take OTC antihistamines?
Children under 6 should not take first-generation antihistamines like Benadryl. For kids 2 and older, non-sedating options like children’s Zyrtec or Claritin are approved, but always follow the label for weight-based dosing. Talk to a pediatrician before giving any antihistamine to a child under 2.
Do antihistamines lose effectiveness over time?
There’s no strong evidence that antihistamines stop working with long-term use. If your symptoms return, it’s more likely due to increased allergen exposure or a change in your immune response. Switching between different antihistamines can sometimes help if one seems less effective.
What’s the difference between Allegra and Allegra-D?
Allegra contains only fexofenadine, an antihistamine. Allegra-D adds pseudoephedrine, a decongestant. Use Allegra-D only if you have nasal congestion. The decongestant can raise blood pressure and cause insomnia, so it’s not for everyone. Stick with plain Allegra if you just need allergy relief.
What’s Next?
If you’ve tried a few antihistamines and still struggle, consider seeing an allergist. They can test for specific triggers and recommend targeted treatments - like nasal sprays, eye drops, or immunotherapy. For most people, though, the right OTC antihistamine is all they need.
The key is matching the drug to your life. If you drive for a living, pick Allegra. If you need quick relief and don’t mind a nap, Benadryl at night is fine. For daily, reliable relief without the fog, Claritin and Zyrtec are solid choices.
Antihistamines aren’t magic - but when used wisely, they turn unbearable allergy season into something you can manage, day after day.




Andrew Forthmuller
November 13, 2025 AT 15:13Allegra ftw. No drowsiness, just relief.
Elizabeth Buján
November 13, 2025 AT 19:26I used to swear by Benadryl until I tried driving after taking it-felt like I was underwater. Zyrtec made me nap at my desk. Then I tried Allegra and it was like my brain finally woke up. Honestly? Life-changing. I wish I’d known this sooner.
vanessa k
November 14, 2025 AT 12:07So many people don’t realize how dangerous first-gen antihistamines are for older adults. My grandma took Benadryl every night for ‘sleep’ and started stumbling around the house. She didn’t even know it was the meds. This post saved her from a fall.
Arpita Shukla
November 14, 2025 AT 19:52Actually, most of this is common knowledge in pharmacology circles. The blood-brain barrier penetration data is well-documented since the 90s. And yes, grapefruit juice interacts with fexofenadine-but that’s true for like 47 other drugs too. People act like this is groundbreaking when it’s just textbook material.
manish kumar
November 16, 2025 AT 04:34As someone from India where allergy season is brutal and OTC meds are often unregulated, I can say this guide is spot-on. We don’t have access to Allegra everywhere here, but when we do, it’s the only one that lets me work in the office without falling asleep. Also, never mix with chai-too much caffeine + antihistamine = jittery nightmare.
Charles Lewis
November 17, 2025 AT 04:39It is imperative to underscore that the pharmacodynamic distinctions between first-generation and second-generation H1 antagonists are not merely clinical curiosities-they represent a fundamental evolution in therapeutic safety profiles. The cognitive impairment associated with lipophilic compounds such as diphenhydramine, which readily cross the blood-brain barrier, has been quantified in multiple double-blind, placebo-controlled trials, demonstrating significant decrements in psychomotor performance comparable to legally intoxicated states. Conversely, the hydrophilic nature of fexofenadine renders it incapable of substantial CNS penetration, thereby preserving executive function and occupational safety. This is not anecdotal; it is evidence-based medicine at its most pragmatic.
Samantha Wade
November 18, 2025 AT 22:18I appreciate how thorough this is, but I want to add something critical: don’t assume ‘non-sedating’ means ‘no side effects.’ Dry mouth, headache, and GI upset are real-and they’re often dismissed. I’ve seen patients quit Zyrtec because they thought ‘it wasn’t working’ when really, they were just dehydrated and irritable from constant dry mouth. Drink water. Use a humidifier. And if you’re on it daily for months, get your electrolytes checked. This isn’t just about sleepiness-it’s about holistic wellness.
Benjamin Stöffler
November 20, 2025 AT 21:15But… what if… the real issue isn’t the antihistamine… but the fact that we’ve normalized living in a world where our immune systems are constantly under siege by industrialized pollen, plastic dust, and glyphosate-laced air? Are we treating symptoms… or avoiding the root cause? I mean, have you ever considered… that maybe your allergies are a cry for a different life? A slower life? Less screens? More dirt under your nails? The body knows. The body remembers. The body… is trying to tell you something.
Nicole M
November 22, 2025 AT 07:29Wait so does Allegra-D count as an antihistamine? Or is the decongestant the main thing? I always get confused because the box says ‘allergy + congestion’ but I just want the allergy part.
Mark Rutkowski
November 23, 2025 AT 02:42There’s a quiet poetry in how our bodies react to pollen-like nature’s way of reminding us we’re not separate from the world, just passing through it. Allegra doesn’t just block histamine; it lets you breathe again. And in a world that’s always screaming, sometimes the most radical thing you can do is simply… inhale. Without fear. Without fog. Just air. And that? That’s peace.
Ryan Everhart
November 23, 2025 AT 07:48Wow. A whole article about antihistamines and not a single mention of the fact that people who take these daily are basically paying Big Pharma to let them keep living in a moldy apartment with 12 cats and no air filter. Just saying.
Renee Ruth
November 24, 2025 AT 21:53So Zyrtec makes you sleepy? Of course it does. It’s the one everyone takes because they’re too lazy to read the label. And now they’re mad when they crash at 3 p.m. and blame the medicine. Meanwhile, I’m on Allegra, working my 10-hour shift, and my coworker thinks I’m a robot. Honestly? I’m just the one who did the research.