Blood pressure: simple, practical steps to lower and control it
High blood pressure raises the chance of heart attack, stroke, and kidney problems. You don’t need a perfect plan—small, steady changes work. Read on for quick, useful actions you can start today and plain language about medicine options so you know what to ask your clinician.
Measure it right. Sit quietly for five minutes, feet on the floor, arm supported at heart level. Use a validated arm cuff and take two readings, one minute apart. Record both. Tracking daily or weekly trends tells you more than a single number at the clinic.
Move more, even in short bursts. Try 30 minutes of moderate activity most days—brisk walking, cycling, or a home workout. If 30 minutes straight feels hard, split it into three 10-minute sessions. Exercise helps blood pressure, mood, and weight.
Cut the hidden salt. Many packaged foods hide sodium: canned soups, deli meat, sauces. Aim for under 2,300 mg sodium per day; lower if your doctor recommends it. Cook more at home and flavor food with herbs, garlic, and lemon instead of salt.
Pick blood-pressure-friendly foods. Vegetables, fruit, whole grains, beans, fish, and low-fat dairy help. The DASH-style pattern—more potassium-rich foods and less saturated fat and sugar—lowers pressure for many people. Swap sugary snacks for fruit and choose whole grains over refined ones.
Lose a little weight if you need to. Dropping 5–10% of body weight often lowers blood pressure. Set small, realistic goals and focus on steady habits—regular meals, fewer sugary drinks, and more movement.
Mind alcohol, caffeine, stress, and sleep. Keep alcohol within recommended limits. If caffeine spikes your readings, try testing before and after coffee. For stress, try short breathing exercises or a quick walk. Poor sleep or loud snoring may mean sleep apnea, which raises blood pressure—ask your doctor about testing.
When medication is needed
Many people also need medicine. Common classes include ACE inhibitors, ARBs (for example Avapro/irbesartan), diuretics (water pills), calcium channel blockers, and beta blockers. Each has trade-offs. For example, ACE inhibitors and ARBs can affect kidney function and potassium, so labs are needed after starting them. Talk openly with your clinician about side effects and costs—there are usually alternative options if one drug doesn’t suit you.
Safety, monitoring, and buying meds
Check labs as your doctor advises (kidney tests, potassium). Don’t stop meds suddenly. If cost is an issue, ask about generics or patient assistance. If you order medicines online, use licensed pharmacies and avoid sites that sell without a prescription. The site’s guides on buying Avapro or choosing Lasix alternatives can help you spot safe pharmacies and common red flags.
Seek urgent care if you get severe headache, chest pain, shortness of breath, sudden vision changes, or very high readings over 180/120—those may signal an emergency. For everyday control, focus on steady tracking, one habit change at a time, and regular follow-ups with your clinician. Small consistent steps add up fast.
 27 April 2023
27 April 2023
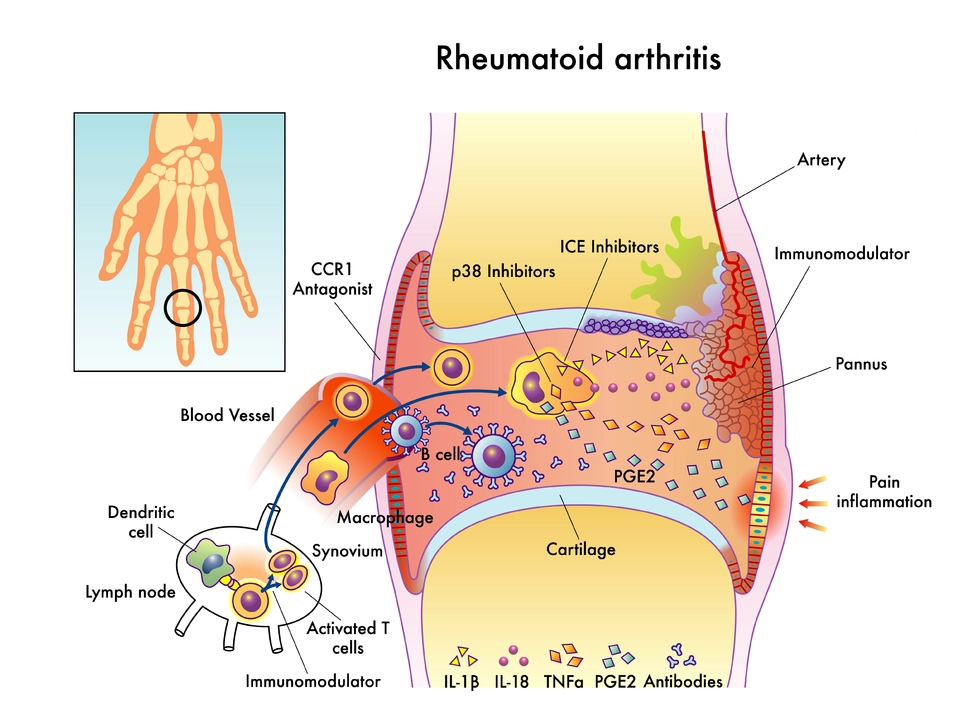
The Impact of Azilsartan on Blood Pressure in Patients with Rheumatoid Arthritis
As a copywriter, I recently came across an interesting study on the impact of Azilsartan on blood pressure in patients with rheumatoid arthritis. It turns out that this medication can significantly help in managing high blood pressure, which is a common issue for those suffering from rheumatoid arthritis. By effectively lowering blood pressure, Azilsartan can not only reduce the risk of cardiovascular complications but also improve the overall quality of life. I'm glad to know that there are treatments like this available to help those living with rheumatoid arthritis. It's essential to spread awareness about such medications and their benefits so that more patients can live healthier lives.
Latest Posts
-

Hatch-Waxman Act: How It Shaped Generic Drug Access in the U.S.
-

Personal Health Records: How to Manage Medications Across Pharmacies
-

A‑Ret Gel vs Other Tretinoin Treatments: Complete Comparison
-

Inactive Ingredient Interactions in Generic Medication Combinations
-

Bloating after a meal: the importance of a balanced gut microbiome

13