Abdominal Pain Liver Connection: What You Need to Know
When talking about abdominal pain liver connection, the relationship between discomfort in the upper belly and liver health. Also known as upper abdominal liver pain, this link helps doctors figure out whether a tummy ache signals a liver problem or something else. Understanding it saves time, cuts down on unnecessary tests, and gets you the right care faster.
The core of the issue often ties back to liver disease, any condition that harms liver cells or blocks its function. When the liver is inflamed, scarred, or overloaded, it can send pain signals straight to the diaphragm and the upper abdomen. Another frequent player is the gallbladder, a small organ that stores bile and can cause sharp right‑side pain if stones form. Finally, hepatitis, viral or autoimmune inflammation of the liver, often shows up as a dull ache, fatigue, and jaundice. These three entities—liver disease, gallbladder problems, and hepatitis—form the main triangle that shapes the abdominal pain liver connection.
How the Connection Shows Up in Real Life
People usually notice a vague, burning feeling right under the rib cage. The pain may worsen after a heavy meal, alcohol, or a night of drinking. If the liver is struggling, you might also see dark urine, pale stools, or a yellow tint to the skin—classic signs of impaired liver function. Elevated liver enzymes in blood tests (ALT, AST, ALP) often confirm that the organ is under stress. On the other hand, gallbladder‑related pain spikes after fatty foods and can radiate to the right shoulder. Distinguishing between these cues is crucial because treatments differ: liver disease may need antiviral meds, lifestyle changes, or even transplant evaluation, while gallbladder stones often require a simple surgical procedure.
Medication side effects are another hidden factor. Many prescription drugs—like certain antibiotics, anticoagulants, and even some cholesterol‑lowering pills—can raise liver enzymes or trigger inflammation. If you’ve started a new medication and notice abdominal discomfort, it’s worth checking whether that drug has a known impact on liver health. This is why the tag collection includes articles on drugs such as warfarin, lactulose, and various antibiotics, all of which can intersect with liver function.
Diagnosis usually starts with a thorough history and physical exam. Doctors listen for tenderness in the right upper quadrant and may order an ultrasound to visualize the liver and gallbladder. If the imaging is unclear, a CT scan or MRI provides a deeper look. Blood work, especially a full liver panel, helps pinpoint the exact cause—whether it’s viral hepatitis, non‑alcoholic fatty liver disease, or a blockage caused by gallstones.
Managing the abdominal pain liver connection starts with addressing the root cause. For liver disease, lifestyle tweaks—cutting back on alcohol, adopting a Mediterranean‑style diet, and regular exercise—can lower liver fat and improve enzyme levels. Hepatitis patients benefit from antiviral therapy and vaccination to prevent future infections. When gallbladder stones are the culprit, a cholecystectomy often resolves the pain permanently. In all cases, staying hydrated, avoiding overly fatty meals, and monitoring medication side effects are practical steps you can take right now.
Remember, persistent upper‑abdominal pain isn’t something to ignore. It could be the body’s way of telling you that your liver or gallbladder needs attention. The articles below explore specific drugs, supplements, and health conditions that can influence this connection, giving you a deeper dive into each scenario. Keep reading to discover how common medications, dietary choices, and lifestyle habits intersect with the abdominal pain liver connection and what you can do to stay ahead of potential problems.
 1 October 2025
1 October 2025
How Severe Stomach Pain Can Signal Liver Disease
Learn how severe stomach pain can signal liver disease, explore common liver conditions, diagnostic steps, and when to seek medical help.
Latest Posts
-
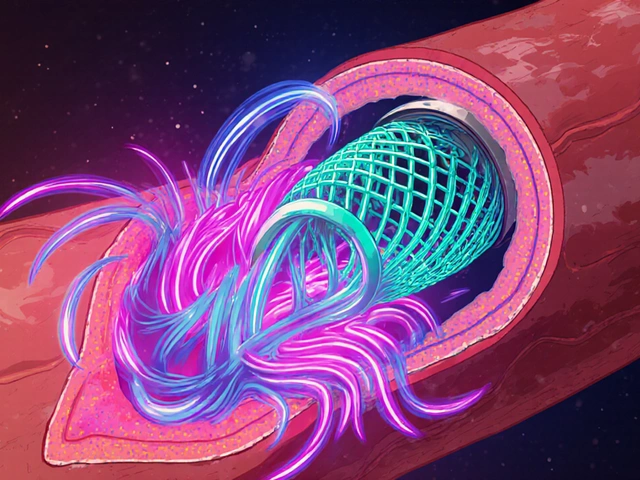
How High Blood Pressure Increases Risk of Blood Clots in Stents
-

The Crucial Role of Fluconazole in Managing HIV/AIDS
-

Travel Sickness and the Elderly: Caregiver Tips for a Smooth Journey
-
Experience the Magic of Delphinium: The Dietary Supplement That's Taking the Wellness World by Storm
-

Meniscus and ACL Injuries: Understanding Knee Pain and When Surgery Is Needed

13