What Is Pancreatitis, Really?
Think of your pancreas as a quiet factory tucked behind your stomach. It makes enzymes to break down food and hormones like insulin to control blood sugar. When it gets inflamed-called pancreatitis-that factory starts attacking itself. The enzymes it normally releases into the gut turn inward, digesting the pancreas from the inside out. This isn’t just stomach upset. It’s serious, sometimes life-threatening, and the way it hits you depends on whether it’s acute or chronic.
Acute Pancreatitis: The Sudden Crisis
Acute pancreatitis comes on fast. One day you’re fine; the next, you’re doubled over with severe pain in your upper belly that shoots straight through to your back. Nausea, vomiting, fever-it hits like a storm. About 80% of cases are mild and clear up in a few days with rest, fluids, and no food for a short time. But 20% go bad fast. If the inflammation triggers organ failure-like your kidneys or lungs stopping-mortality can jump to 15-30%.
Doctors diagnose it with three things: pain that fits, blood tests showing lipase or amylase levels more than three times normal, and imaging (like a CT scan) showing swelling or fluid around the pancreas. The most common causes? Gallstones and alcohol. Together, they cause about 70% of cases. Other triggers include high triglycerides, certain medications, and, surprisingly, about 20% of cases have no clear cause-called idiopathic.
Chronic Pancreatitis: The Slow Burn
Chronic pancreatitis isn’t a single event. It’s damage that piles up over years. Think of it like scarring on your pancreas from repeated attacks. The tissue turns hard, calcified, and loses function. Pain becomes a constant companion, often worse after eating. But here’s the twist: over time, the pain may actually get less intense. That’s not a good sign. It means the pancreas is running out of cells to hurt-it’s failing.
By the time someone reaches the late stage, 90% have lost the ability to make digestive enzymes, and half will develop diabetes. Alcohol is the main culprit in 80% of cases, but genetics play a role too. Mutations in genes like PRSS1 or CFTR can make some people far more vulnerable. Smoking? It doesn’t just add risk-it speeds up the damage. Quitting smoking is the single most effective way to slow progression.
How They’re Different: A Quick Side-by-Side
| Feature | Acute Pancreatitis | Chronic Pancreatitis |
|---|---|---|
| Onset | Sudden, severe | Gradual, often recurring |
| Pain pattern | Constant, radiates to back | Post-meal, dull or sharp |
| Lab marker | Lipase >3x normal | Normal or only slightly elevated |
| Imaging signs | Pancreatic swelling, fluid | Calcifications, duct widening |
| Recovery | Most recover fully | Permanent damage, progressive |
| Long-term risks | Organ failure, infection | Diabetes, malnutrition, pancreatic cancer |

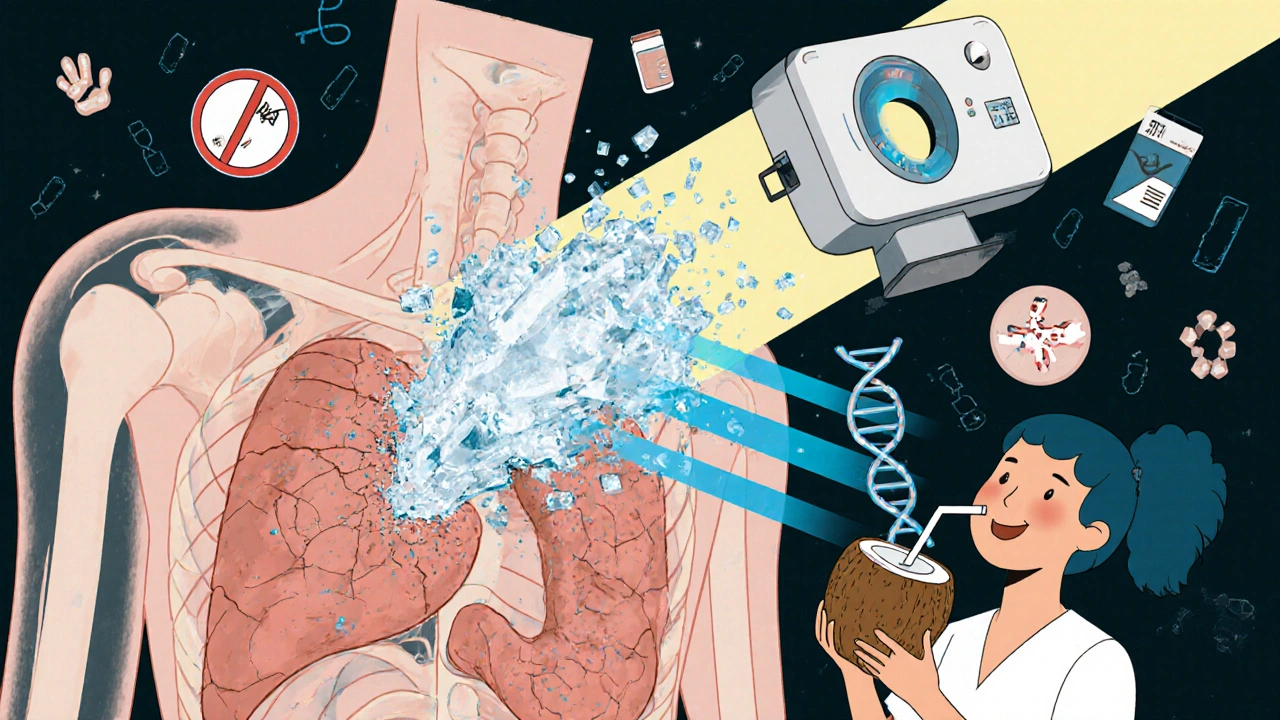
Nutrition in Recovery: It’s Not Just About What You Eat
When you’re in acute pancreatitis, your body needs to rest. That means no food at first-sometimes for days. But here’s the key: don’t wait too long. Starting enteral nutrition (feeding through a tube into the small intestine) within 24-48 hours cuts infection risk by 30%. The goal? Give your gut what it needs without overloading the pancreas.
Once you can eat again, start small. Low-fat, easy-to-digest foods: white rice, boiled chicken, applesauce, toast. Avoid fried food, cream, butter, and alcohol. Even a little fat can trigger pain. Most people bounce back to normal eating within a week-unless they have a second attack.
Chronic Pancreatitis Nutrition: A Lifelong Strategy
With chronic pancreatitis, nutrition isn’t temporary. It’s your main tool for survival. Your pancreas can’t make enzymes anymore, so you need replacements. That’s pancreatic enzyme replacement therapy (PERT). Dosing? 40,000-90,000 lipase units with meals, 25,000 with snacks. Take them right before you eat. If you take them too late, they won’t work.
But here’s the catch: many people don’t take enough. Or they take them with water instead of with food. Or they skip snacks. Result? Fatty stools, weight loss, vitamin deficiencies. Studies show 85% of chronic patients are low in vitamin D, 40% in B12, and 25% in vitamin A. These aren’t just numbers-they mean weak bones, nerve damage, and poor immunity.
Medium-chain triglycerides (MCTs) are a game-changer. Unlike regular fats, MCTs don’t need pancreatic enzymes to be absorbed. Found in coconut oil and special medical formulas, they give you calories without triggering pain or malabsorption. Many patients report fewer bowel movements and better energy after switching.
Meal timing matters too. Six to eight small meals a day beat three big ones. It keeps blood sugar steady, reduces pressure on the pancreas, and helps with digestion. Avoid sugar spikes-you’re at risk for pancreatogenic diabetes, which behaves differently than type 1 or 2. That’s why new continuous glucose monitors (like Dexcom G7) are now approved specifically for these patients.
What Doesn’t Work (And What Does)
Don’t fall for the myth that “eating less fat forever” is the answer. In chronic pancreatitis, you need fat-but the right kind. Total fat should be 40-50 grams per day, not zero. Too little fat means you’re missing out on essential nutrients and calories. You’ll lose weight, get weaker, and feel worse.
Probiotics? Emerging evidence shows certain strains-like Lactobacillus rhamnosus GG and Bifidobacterium lactis-can reduce pain by 40% over six months. Not a cure, but a helpful support. And yes, quitting smoking cuts disease progression by half. No other intervention comes close.
Alcohol? Stop. Full stop. Even if you think you’re “only having a glass.” For chronic pancreatitis, there’s no safe amount. The damage is cumulative. Hair tests show fatty acid ethyl esters in 90% of cases linked to alcohol-proof your body is still reacting to past exposure.
The Hidden Risks Nobody Talks About
Chronic pancreatitis doesn’t just mess with digestion. It raises your risk of pancreatic cancer by 15-20 times. The 10-year risk? About 4%. That’s why high-risk patients-especially those with genetic mutations or long-standing disease-are now being screened with annual MRI or MRCP scans. Early detection saves lives.
And then there’s pain. It’s not just physical. Many patients end up on opioids. Studies show 30% develop dependence within five years. That’s why multidisciplinary care matters: pain specialists, nutritionists, endocrinologists, and mental health support all in one team. Patients who get this kind of care report better quality of life and fewer hospital visits.
What Recovery Really Looks Like
Recovery from acute pancreatitis? Most people go back to normal. No long-term issues. But if you’ve had one episode, you’re at higher risk for another. Avoid alcohol, manage triglycerides, and watch your weight.
Recovery from chronic pancreatitis isn’t about getting better. It’s about managing decline. It’s about taking enzymes every meal, getting blood tests for vitamins, eating small meals, staying off alcohol and cigarettes, and monitoring your blood sugar. It’s hard. It’s exhausting. But it works.
A patient in her 50s told her doctor: “I used to dread breakfast. Now I eat oatmeal with MCT oil, take my enzymes, and feel like I can breathe again.” That’s not magic. That’s science. That’s nutrition done right.
Frequently Asked Questions
Can you fully recover from acute pancreatitis?
Yes, most people do. Around 80% of acute pancreatitis cases resolve completely within a week with proper care-rest, fluids, and avoiding triggers like alcohol or fatty foods. But if you’ve had one episode, your risk of another goes up. Preventing recurrence means identifying and managing the cause-whether it’s gallstones, high triglycerides, or alcohol.
Do I need to take pancreatic enzymes forever if I have chronic pancreatitis?
Almost always, yes. Once your pancreas stops making enough enzymes, your body can’t digest fats, proteins, or carbs properly. Enzyme replacement therapy (PERT) is lifelong. Dosing varies by meal size and fat content-typically 40,000-90,000 lipase units per main meal. If you still have greasy stools or unexplained weight loss, your dose may need adjusting. Always take them right before eating.
Why do I still lose weight even though I’m taking enzymes?
There are a few reasons. First, you might not be taking enough enzymes-or not taking them at the right time. Second, your diet might still be too high in fat. Third, you could be low in stomach acid, which affects how well enzymes work. Fourth, you might have vitamin deficiencies (like B12 or D) that affect metabolism. A 72-hour fecal fat test can confirm if enzymes are working. If not, your doctor may adjust your dose or add acid-reducing meds.
Is it safe to drink alcohol after having pancreatitis?
No. Even one drink can trigger another attack of acute pancreatitis. For chronic pancreatitis, alcohol accelerates tissue damage and increases cancer risk. Studies show that continuing to drink after diagnosis cuts survival time in half. Abstinence is non-negotiable. There is no safe level of alcohol for someone with pancreatitis.
Can diet alone manage chronic pancreatitis without enzymes?
No. While a low-fat, nutrient-rich diet helps, it can’t replace the enzymes your pancreas no longer makes. Without enzyme replacement, you’ll continue to malabsorb fats and fat-soluble vitamins (A, D, E, K), leading to weight loss, bone loss, vision problems, and immune weakness. Diet supports treatment-it doesn’t replace it.
What’s the link between chronic pancreatitis and diabetes?
Chronic pancreatitis damages the insulin-producing cells in the pancreas. About 50% of patients develop diabetes within 12 years. This isn’t type 1 or type 2-it’s called pancreatogenic diabetes (type 3c). It’s harder to manage because insulin needs change quickly, and blood sugar swings wildly. Continuous glucose monitors designed for this type of diabetes can help track those patterns and guide treatment.
Should I be screened for pancreatic cancer if I have chronic pancreatitis?
Yes-if you’ve had chronic pancreatitis for more than 5 years, especially if you smoke, drink, or have a family history. Your risk is 15-20 times higher than average. Annual MRI or MRCP scans are recommended for high-risk patients. Early detection is critical because pancreatic cancer is often caught too late. Talk to your gastroenterologist about a surveillance plan.
Next Steps for Managing Pancreatitis
If you’ve been diagnosed with acute pancreatitis: focus on recovery. Avoid alcohol. Get checked for gallstones. Monitor your triglycerides. Eat clean, low-fat meals. Follow up with your doctor in 4-6 weeks.
If you have chronic pancreatitis: build a team. Find a gastroenterologist who specializes in pancreas disorders. Get on pancreatic enzyme therapy. Test for vitamin deficiencies. Quit smoking. Eat small, frequent meals with MCT oil. Monitor your blood sugar. Ask about annual imaging. Don’t try to manage this alone-it’s too complex.
Pancreatitis isn’t just a digestive issue. It’s a whole-body condition. Nutrition isn’t a side note-it’s the backbone of survival. Get it right, and you can live well-even with a damaged pancreas.




Prem Hungry
November 17, 2025 AT 23:30man i had this last year after binge drinking at a wedding... thought it was just food poisoning. turned out my pancreas was screaming. doc said no more alcohol, ever. now i drink coconut water with MCT oil instead. life’s weird but better. 🙌
Leslie Douglas-Churchwell
November 19, 2025 AT 19:53Let’s be real - the pharmaceutical-industrial complex is profiting off your enzyme dependency. PERT? It’s a $20,000/year racket. Meanwhile, the FDA suppresses natural alternatives like pancreatic glandular extracts from grass-fed bovines. And don’t get me started on how glyphosate in your oatmeal is accelerating pancreatic fibrosis. 🌱💊📉
shubham seth
November 20, 2025 AT 23:20bro the real villain isn't alcohol - it's the goddamn food industry pushing processed fats and high-fructose corn syrup into everything. pancreas doesn't care about your ‘low-fat’ diet if it's laced with carrageenan and soybean oil. i went from 180lbs to 120lbs in 6 months because i ate nothing but boiled eggs, white rice, and MCT oil like some kind of biohacking monk. my stools? clean. my energy? nuclear. my doc? confused.
Kathryn Ware
November 21, 2025 AT 02:38I’m a registered dietitian specializing in GI disorders, and I want to say thank you for this incredibly thorough breakdown. So many patients think ‘no fat’ means ‘healthy’ - but it’s the opposite. Without adequate fat intake, especially MCTs, you risk muscle wasting and micronutrient collapse. I always recommend starting with 1 tsp of coconut oil per meal and gradually increasing. Also - vitamin D levels? Non-negotiable. Get them checked quarterly. And yes, L. rhamnosus GG has real data behind it - I’ve seen patients cut opioid use by half just by adding a probiotic. You’re not alone in this. 🌿💪❤️
kora ortiz
November 21, 2025 AT 13:54Stop overcomplicating this. No alcohol. No smoking. Take enzymes before every bite. Eat small meals. Test your vitamins. Screen for cancer. Do it or die trying. Simple. Not easy. But simple. I’ve seen too many people die because they listened to influencers instead of science. Your pancreas doesn’t care about your TikTok diet trends. Get it right.
Jeremy Hernandez
November 21, 2025 AT 18:43LMAO look at all these ‘experts’ acting like they’re saving lives. Meanwhile, the real cause of pancreatitis? Corporate greed. Big Pharma sells you enzymes. Big Food sells you the fat that kills you. Big Insurance won’t cover MRCP scans unless you’re dying. And the doc? He’s got 7 minutes per patient. You think this is medicine? Nah. It’s a survival game. And you’re playing with loaded dice.
Tarryne Rolle
November 23, 2025 AT 09:46Isn’t it ironic that we treat the pancreas like a broken machine that needs parts replaced - when really, it’s a sentient organ that’s been screaming for decades? We don’t heal it. We manage its suffering. We weaponize nutrition as control. We call it ‘recovery’ when it’s just prolonged resignation. What if the answer isn’t more enzymes… but less guilt? Less fear? Less human arrogance about controlling biology?
Kyle Swatt
November 24, 2025 AT 05:29I lost my dad to this. He was a 60-year-old mechanic who drank one beer a night for 40 years. Thought he was fine. Then one day he couldn’t stand up. They told him to quit alcohol. He did. Took enzymes. Ate clean. But the damage? It didn’t care. The cancer came three years later. They gave him six months. He lasted 11. He never complained. Just ate his oatmeal with coconut oil, smiled, and said ‘at least I didn’t die drunk.’ I don’t know if this post saves lives. But I know it honors them. Thanks for writing this. I’ll share it with every family I know.